SUBSCRIBE TO BIG MED AT THE BIG MED SITE ON GOOGLE GROUPS.

November 10, 2009
| AMERICAS | OCEANIA | EUROPE | MIDDLE EAST | ASIA | POLITICS | BUSINESS | RESEARCH | EDUCATION | WORKFORCE |
Big Medicine is published by Team EMS Inc.
Managing Editor
Contact: ideas@tems.ca
Views
Contributor Emeritus
Tools
Stop Violence Against Women & Girls
The views expressed here reflect the views of the authors alone, and do not necessarily reflect the views of any of their organizations. In particular, the views expressed here do not necessarily reflect those of Big Medicine, nor any member of Team EMS Inc.
VIEWS: JIM RUSH
The healthcare supply system and emergency management
[October 19 2009]
Purchasing, Managing and Distributing Federal Reserve Inventories
Elected officials, emergency managers, healthcare executives and public health officials are focused on protecting and treating patients who are, or will be infected by the H1N1 epidemic.
Government procurement officials now understand that all the money in the world can’t buy medical products that are unavailable due to high worldwide demand. The government also is recognizing that when worldwide demand for any commodity is very high, the supply chain simply cannot keep up with orders. It is becoming very clear that governments need to build reserve inventories to accommodate sudden spikes in demand.
Currently, there is less understanding that if hospital admissions surge, there will be shortages not only for obvious products like anti-viral medicines, N-95 respirators and isolation gowns, but for every item hospitals use in treating seriously ill patients.
Thus, I thought I’d suggest a methodology of proactive purchasing, managing and distributing America’s emergency relief supplies in meaningful quantities to sustain the healthcare industry and community mass care facilities during large-scale, long duration disasters.
This recommended system uses professional supply chain managers, healthcare distributers and logistics companies to purchase, manage, transport, distribute and account for Federal relief supplies, equipment and vaccines.
The first thing we need to realize is there are two very different management approaches to acquiring and distributing medical materiel.
The second thing to realize is that the Private Sector Healthcare Supply Chain manages Just-In-Time inventories for normal medical product demand and there are no meaningful medical reserve inventories to supplement and sustain the Healthcare Industry during extraordinary spikes in demand for supplies, equipment or services.
1. Just-In-Time (JIT). The Private Sector healthcare supply chain managers do a great job in predicting the demand for medical materiel during normal times. During the past 30 years, supply chain computer models have become extremely accurate in predicting supply usage; locally, regionally and nationally. While “predictive computer demand models” can predict seasonal spikes in demand for medical items which are “cold and flu” season- based, no computer can predict spikes in demand for medical material for disasters and epidemics. This means in the Public Sector, there are no “Just in Case” Reserve Inventories of supplies, equipment or vaccines. America has a Strategic National Stockpile (SNS), designed to assist Public Health departments as they respond to public health needs, but the SNS was never designed to support and sustain America’s Healthcare Supply Chain. The difference between normal medical product consumption rates of medical materiel and the consumption rates associated with a large-scale disaster is astounding. From a National perspective, patient admissions are currently modestly elevated as compared with a normal influenza season. While there are backorders for selected medical products, these outages are manageable, at least over the short term. On the other hand, if we see a 50%-100% increase in seasonally adjusted patient admissions over time, the healthcare industry’s supply chain may not be elastic enough to surge manufacturing in time to meet the demand. It is becoming more and more obvious that the Government must plan to supplement medical materiel inventories for use by healthcare organizations during large scale and long term disasters. For maximum value and usefulness, these inventories should be purchased by the Federal Government under the Emergency Support Function (ESF)-8, Health and Medical Services, or ESF-6 Mass Care, Housing, and Human Services as described in the National Response Framework. It is less important which ESF Agency purchases, manages and distributes disaster-related medical materiel than it is to have serviceable medical products and services available when needed.
2. Reserve Inventories. Elected and appointed National leaders need to understand that “Preparing for unpredictable spikes in demand for medical items is predominately a Government responsibility.” Certainly, the Private Sector healthcare industry can help Federal planners develop stock listings of every medical supply and every item of equipment that will be needed during each planning scenario. This process is called “requirements development” and although it’s a bit tedious, requirements development is very easy to do. Developing requirements is easy but purchasing the medical materials and managing very high quantities of many individual supply line items without losing any items to expiration in storage, takes significant expertise and time. The good news is that healthcare distributors are among the best in the world at managing medical materials in storage and at moving those materials where and when they are needed. The only issues remaining are “who is going to purchase disaster-related medical materials” and “who is going to pay to manage these large inventories while they are held in reserve for future disasters.” The answer is easy, since Private Sector business cannot invest in inventories which exceed normal demand; the Federal Government must invest in Federal Reserve Inventories (FRI).
This does not mean that the Government needs to set up a parallel healthcare supply chain. Remember the healthcare supply chain is extraordinarily efficient at getting supplies and equipment from the manufacturer’s loading dock to healthcare organizations and retailers wherever they are needed. More importantly, the velocity of medical supplies flowing through the supply pipeline each and every day means the healthcare supply chain can rotate huge quantities of FRI if the Government would just purchase it.
The Federal Government, under either HHS under Emergency Support Function (ESF)-8 Health and Medical, or FEMA under ESF-6, should purchase FRI and entrust its management to Healthcare Distributors to manage and distribute it when authorized. Hopefully, the Department of Homeland Security (DHS) will determine which agency must support the FRI soon. For the purpose of this article, Federal Agencies will be referred to as “The Fed.”
By developing a FRI system, The Fed will assist healthcare and public health practitioners:
o Save lives
o Save money
o Meet the 48 hour HHS post-exposure mass prophylaxis requirement
o Improve stewardship of a National asset
o Improve operations, inventory tracking and asset visibility
o Reduce “in-transit” time to the affected jurisdiction’s healthcare organizations
o Facilitate much faster dispensing and vaccination
o Improve Public Health response
o Improve citizen acceptance
Managing and Distributing Federal Reserve Inventories (FRI) of Vaccines, Medical Supplies
1. Concept of Operations: The Fed will use established, mature and proven Healthcare Distributor Supply Chains to store, manage (stock rotation and quality control), and rapidly distribute and account for all FRI materiel during declared disasters or public health emergencies.
A. During normal operations: The Fed maintains oversight of all government owned materiel. They also develop and share with distributors, a list of participating dispensing centers/immunization centers, as well as Public Health and healthcare entities to be supplied with FRI materials during a disaster. Maximum order quantities and other formulas such as “priority dispensing entities” can be established during this period.
B. During Disasters: Upon requests from jurisdictional officials, The Fed releases FRI materiel into the appropriate healthcare distributors supply chains for distribution to the healthcare or public health entities requesting FRI.
C. Post Disaster Accountability: The Fed and the receiving jurisdiction’s chief fiscal officer obtains reports from distributors regarding which entities received FRI materiel by line item and dollar value.
(1) Distributor-provided FRI usage lists will serve as documentation for The Fed to request FRI replenishment dollars from Congress.
(2) The Fed will be able to quickly and easily develop post-disaster activity and accountability reports
2. Why use existing supply chains and logistics networks?
A. Healthcare Distributors have the knowledge, competency and experience of moving millions of dollars in medical pharmaceuticals, vaccines, medical materiel from manufacturers to customers every day.
B. Defense Logistics Agency (DLA) and the Department of Veterans Affairs (VA) and HHS’ Supply Service Center have already established Prime Vendor relationships with the Nation’s major pharmaceutical and medical surgical distributors-the framework is in place.
C. Distributor supply chains are already established and can do the job in an emergency.
D. All customers’ addresses are already in the distributors’ system, so the interface for sustainment during disasters will be seamless.
E. Distributors will be out of their normal operating stock during the disaster-related spike in demand. The Distributors’ workforce can then distribute FRI stock instead of closing shop.
F. During normal operations, manufacturer supplies flow through this pipeline- the FRI materials can flow through the pipeline just as smoothly.
G. Distributors have highly developed supplier relationships with:
(1) Pharmacy chains-Walgreen’s, Eckerd, CVS, etc.
(2) Public health clinics
(3) Military and VA hospitals and medical centers
(4) Hospitals and medical centers
(5) Nursing homes
(6) Assisted living communities
(7) Neighborhood health centers & urgent care centers
(8) Prison healthcare centers
H. Distributors have highly refined systems to interface with logistics and transportation companies and maintain long-standing relationships with:
(1) UPS
(2) FedEx
(3) Many other National and International logistics companies
(4) Hundreds of other independent short and long-haul freight companies
(5) Thousands of courier services
(6) The FED should leverage this existing experience to obtain fastest point-to-point service during disasters.
Dispensing:
1. Concept of Operations: Since the vast majority of Americans know where they normally get their medicines, use pharmacies for dispensing and physician offices and public health departments for vaccinations as the 1st tiers of the dispensing and immunization systems.
2. Why use the existing pharmacies as the disaster dispensing network?
A. Pharmacists know their clients
B. Pharmacies maintain automated records for all patients served in order to discover medication errors, contraindications, allergies etc.
C. Pharmacies are tied into distributor networks and have alternate distributor arrangements if one is out of stock.
D. Pharmacists know most of their clients’ family’s medical histories-this enables one family member to pick up courses of treatment for the entire family.
E. Pharmacies can provide numbers of clients served, number of courses of treatment filled, age mix etc., for post-event epidemiological studies.
F. Physician offices routinely provide immunizations and know those most in need
G. Physicians know their patient populations and can best prioritize which patients get immunizations first.
Public Health Departments can manage the event from a Public Health and not a distribution prospective.
1. Public health “At Risk” populations will receive better and more focused care, when the major portion of the population is being served through pharmacies, physician offices and other Healthcare organizations.
2. Public health departments will be unburdened by serving Public Health clinics and facilities only.
3. Public health staff can be utilized in public health activities instead of trying to compete with distributors.
4. Public Health will have more Post-Disaster time to perform studies on the effects of the disaster, instead of reconciling bottles of medicines received to doses/vaccinations given to the entire population.
5. Public Health officials can focus on anomalies and exceptions, instead of trying to manage distribution, dispensing and post event accountability.
6. Public Health personnel are freed to provide a full array of public health services
Results:
1. This initiative will provide better FRI management and distribution using very sophisticated inventory management systems. The FRI will:
A. Remain perpetually fresh with state of the art stock rotation systems.
B. Maintain its identity in storage as “Government Owned Material” (Ownership code “FRI.”
C. Be ready for shipment in minutes-not hours.
D. Be transported through an operationally tested transportation system of ground and air transporters as well as local couriers.
E. Arrive at the right place within the shortest timeframe using established, redundant transportation systems.
F. Get to exposed Americans and to Healthcare organizations within hours.
2. This initiative will also:
A. Meet HHS’s 48 hr. requirement for biological agent post exposure prophylaxis
B. Provide the safest dispensing system for detecting contraindications, allergies etc.
C. Provide timely feedback to FDA on adverse reactions and rapid transmittal of FDA Type I, II and III material complaints
D. Provide better stewardship and accountability.
E. Provide the fastest emergency movement, distribution, and dispensing of lifesaving pharmaceuticals, equipment, supplies and vaccines anywhere they are needed nationally and internationally.
A stimulating idea: Using economic recovery dollars to build disaster healthcare readiness and re-employ workers
by Jim Rush
[July 5 2009]
The American Recovery and Reinvestment Act of 2009, appropriated approximately $787 billion aimed at turning around the American economy during this deep recession. There have been a number of criticisms that these dollars will fall into a number of economic “Black Holes” and provide only temporary results. There is a wonderful alternative.
Recently, I saw a TV interview with Michigan’s Governor Jennifer Granholm discussing the profound downsizing of America’s automobile industry and the devastating effect this is having on countless highly skilled Michigan auto workers. I felt badly for both the Governor and the unemployed Michigan workers. I had the idea that Americans can obtain badly needed mobile disaster hospitals and specialty centers for future disasters, and at the same time put unemployed Michigan workers back to work. Medical Support Equipment and Supplies Manufacturers across America would also benefit. . I have sent a detailed proposal to Governor Granholm and other Michigan elected officials I hope would be interested in this multi-purposed program.
I often wondered if there was a reason why I received very unconventional assignments in my career as a medical logistician. It started in the Air Force and when I left the Service, I remained in Germany, working as an Army civilian employee. I was responsible for supporting medical missions for both war and foreign assistance to Governments overseas during disasters. I was indeed very fortunate in being a part in building mobile medical units. I was even more fortunate in learning from some of the best Medical Readiness people in the Free World.
So what would be the benefits of rebuilding America’s disaster healthcare capabilities using mobile medical assets and support systems?
1. Save lives and lessen suffering. With a well developed mobile healthcare system, we can very quickly reinforce jurisdictions’ Public Health and Healthcare systems when they are in the Response and Recovery stages of a disaster. We all know that victims of hurricanes Katrina, Ike and Gustav had to receive (and many folks still are receiving) healthcare services far away from home.
2. Re-Train and Re-Employ highly skilled workers. My proposed program will train and re-employ tens of thousands of heavy industry and automobile workers in Michigan and in other jurisdictions all across America building mobile medical facilities and support equipment for sustaining these assets during deployment. These facilities and their sustainment packages can be used over and over and will provide long lasting disaster capabilities and enduring jobs during both the manufacturing stage. Afterward, these same workers can be employed in managing these assets in storage, reconstituting hospital and specialty units after each use, repairing equipment, provide maintenance in the field and in transporting and recovering these assets over their 25 years of useful life. The program will also, in fact, be a real and profound stimulus to all manufacturers of medical and support equipment and supplies as well. These mobile medical assets can be sold to our trading partners all over the world and will save countless lives during their many deployments.
3. Stimulate America’s Healthcare Supply Chain. With a real sense of urgency, we can immediately stimulate the healthcare supply chain for medical supplies such as wound, care, burn care, special needs supplies and the full line of medical-surgical consumable supplies. We can also stimulate manufacturers of medical equipment such as surgical and ER equipment, ventilators, patient monitoring equipment, and mobile digital imaging equipment, to name just a few.
4. Use underutilized manufacturing and warehousing facilities idled by the closing automobile manufacturing facilities. Why not re-tool auto plants to begin an entirely new and badly needed manufacture of mobile hospitals, special needs shelters, burn and trauma centers and all the associated support equipment like heavy-duty, long run generators, very high output water purification systems, regulated medical waste treatment equipment and mobile kitchens, just to name a few.
5. Develop the best disaster healthcare system in the world. These units look like hospital wards when they are erected. Sure, they can be augmented by tents for support functions like inventory control/ordering, food service and staff living quarters. But for patients, these facilities are perfect for providing definitive medical care during both the Response and Recovery stages of a disaster. The test I used when selecting these facilities was “Would I feel comfortable with a family member receiving a full continuum of health care including ventilator support in one of these facilities?” The answer was “Definitely.”
6. Provide huge savings to the Taxpayers in future disasters. Yes, savings on top of all the other benefits. Consider the cost of air evacuating patients and family member escorts out of the disaster’s jurisdiction to obtain healthcare at various health centers away from the disaster jurisdiction. That is still happening in Galveston and in some cases, may still be happening in New Orleans. Some entity is paying for this extraordinarily high cost, time-delayed healthcare. These mobile hospitals can be used, reconstituted and redeployed approximately 50 times. They will pay for themselves during their second deployment by providing definitive care instead of only stabilization at locations very near the disaster location. The next 48 deployments will return dollars to America and vastly improve healthcare during Response and Recovery stages. In fact, if we took my suggestion on these units in 2003, Hurricane Katrina and all subsequent hurricane medical responses would have looked far better and infinitely more laudable.
The 1960’s Disaster Healthcare System: During the Cold War, America built a robust Civil Defense Program which included 2,600 Packaged Disaster Hospitals, pre-positioned in strategic locations across America for wartime use.
Each of these packaged disaster hospitals contained 200 beds, a radiology section with a portable X-Ray machine and a 3-table operating suite. Each hospital also had sufficient consumable medical supplies to operate independently for 30 Days. These disaster hospitals gave America 512,000 beds, 7,800 operating rooms and 2,600 radiology sets for surge capacity for disasters or emergencies. Over time, a lack of funding of the Civil Defense program and materials obsolescence resulted in the decay and disposal of the disaster packaged hospitals.
Today, we have none of these capabilities. America has profound shortfalls in medical facilities and associated support capabilities that can be used during disasters.
There are no federal mobile medical assets that can be deployed to jurisdictions during disasters and very limited quantities of pharmaceuticals for biological events..
How can we justify being far less capable of providing healthcare and public health during disasters in 2009 than we were in the 1960’s? We just can’t!
We all know that America’s Healthcare System has been in crisis for over 20 years. A Pandemic, a terrorist attack such as a nuclear detonation in a large population center or any other very large even, will damage and may destroy America’s healthcare system as we know it today. We are seeing a serious lack of health services right now in Galveston, almost a year after hurricane Ike.
We can do the right thing, the compassionate thing and the smart thing by rebuilding our disaster medical system. I hope that all Emergency Managers including those at DHS/FEMA will support this vital initiative by forwarding this paper to their decision makers and supervisors.
Let’s put our fellow Americans to work building a disaster healthcare system capable of saving lives and demonstrating what we can do when we put our minds to it!
Healthcare Disaster Readiness: "The Cost Effectiveness of Good Stewardship"
[May 7 2009]
On the heels of the 24 hour news coverage of the Swine Flu, I began thinking of what it might take to convince healthcare executives to re-examine the idea of “Medical Readiness” from a cost/benefit perspective. Let me lay out the benefits first, since looking on the positive side of this issue first is always best. We’ll get to the costs involved in failure later in the article.
1. Every Healthcare Executive knows that being the best healthcare alternative in their community means-success. Based on that safe assumption, the healthcare executive who has made a commitment to Healthcare Disaster Readiness will reap the following benefits:
a. Available services means revenues: Healthcare Organizations that have developed a “Corporate Culture of Disaster Readiness” will have the best chance of surviving a disaster and remaining profitable during and after the event.
b. FEMA Grant-Ready: Being “Disaster-Ready” also means understanding which types of recovery and/or mitigation assistance the healthcare organization may qualify for during the recovery stage. A thorough understanding of the FEMA Public Assistance (PA) guidance may translate into maximum eligible funding and shorter approval times. Armed with this PA knowledge, the healthcare organization can get back to providing health care, while competitors begin exploring FEMA eligibility criteria and application processes only when FEMA comes to town.
c. Standardization saves money: Healthcare Organizations can reap significant savings by standardizing medical products across the entire Health System and eliminating duplicative products. Fewer medical items (a leaner master item file) can mean better stock levels across the entire supply chain, more aggressive purchasing tiers and far better distributor fill rates during surges in product demand. The Armed Forces learned during the 1991 Gulf War that “preference items” were nothing but trouble for suppliers, medical logisticians and care givers. Private sector healthcare organizations can profit from this experience in more ways than one.
d. Defending the Healthcare Facility is always more cost effective than rebuilding the facility and recruiting new staff. When a healthcare organization fails during a disaster, the staff evacuates with the community and often never returns. The aftermaths of disasters in New Orleans LA and Galveston TX are excellent examples of what happens to healthcare organizations when they cease operations and attempt to rebuild after the disaster.
e. Quicker recovery is good business: The Disaster-Ready Health System will be able to recover much sooner than less prepared competing healthcare organizations. The disaster-ready organization fully understands the steps it needs to take in order to bolster its defenses against disasters and to continue to serve its community during and after a disaster.
f. Patients will trust a disaster-ready healthcare organization over a less dependable one: The CEO knows full well that he/she is a Community Steward for Healthcare Services and must be worthy of the community’s trust. Continuing to serve the community during and after a disaster can only be a positive thing…it can represent a critical competitive advantage.
2. OK, now the negative side of this argument for the less altruistic and those overly-optimistic CEOs who are certain a disaster will not happen to them. These are not bad people and these days keeping the doors open, the lights on and the staff paid, are challenge enough. Still, the consequences of being unprepared can have very dire career consequences for a CEO.
a. Future employment. Consider what the resume of the CEO will look like to future employers when the last Health System he/she led was decimated by a disaster.
b. Insurability. Healthcare insurance companies may take a second look when they discover they are insuring an organization whose CEO’s last healthcare organization failed under the weight of a disaster-especially if mitigation steps could have prevented the failure.
c. CEO-Board of Directors Relations. Imagine the Board of Directors’ reaction to an incoming CEO who let down his/her former Board of Directors by failing to take steps to address vulnerabilities which proved fatal to the facility and thus, the organization.
d. Citizen-Choice. Consider a community which finds itself with a choice between a Disaster-Ready CEO across town and the new CEO arriving from a health system that left his/her community without healthcare.
3. While I am all for using the positive approach in #1 above, it may be time to include both sets of consequences on the tables of Healthcare Organization Board Rooms across America.
Postscript: I once heard a man responsible for Readiness commenting on the consequences of a potential disaster. He said “The worst thing that can happen to me after a disaster is that I’m forced to retire.” I wish I was fast enough on my feet to say to that guy “No, that is not the worst thing that can happen to you….the worst thing that can happen to you is you go through the rest of your life knowing that your inaction and poor stewardship caused many deaths and untold suffering in the community that trusted you to care for its people.”
Being accountable for the community’s healthcare is good stewardship and good business.
Jim Rush
[May 5 2009]
Good Morning: After recently reading and
watching the urgent stories about the Swine Flu, I couldn't help but wonder
how long it would take before we reverted to complacency. For years now, I
have been advocating for a calm, resolute culture of preparedness. Instead,
I have been seeing what I refer to as the PowerGlide of Public sentiment.
For those of you too young to remember, many Chevrolet automobiles in the
60's had a PowerGlide transmission. Low gear and high gear...that's all
there was..... two gears. In the last 8 years, we as a society, have had
only two collective mental gears....complacency and hysteria.
Prior to 9-11 we were in the complacent gear, and afterward, we were scared
to death we would be attacked again and transitioned immediately into the
hysteria gear. Although we all know we are going to be attacked again, soon
after 9-11 we reverted to our complacent gear. As such, we have done little
to significantly improve our overall state of Readiness to manage another
3,000 casualty event, let alone a 100,000-300,000 casualty event such as a
10 Kiloton detonation on a population center or a Pandemic . We just don't
want to think about it.
in 2005, we all saw thousands of people suffering and death during hurricane
Katrina. Folks with disabilities were slumped down dead in wheelchairs
outside storefronts, nurses crying on hospital rooftops while manually
ventilating patients while they waited for a medical evacuation helicopter.
We saw the dead floating down streets in New Orleans-an American city, with
corpses in the water. We are now trying to recover from hurricane Ike in
Galveston and other Texas Coastal towns,,,,and where are we? We are without
healthcare for hundreds of thousands of people, that's where we are.
We have been told by the CDC for years now that it was a matter of "When"
and not "If" we would have a Pandemic. We have a few thousand ill people
around the World who are ill and have experienced far fewer deaths than we
experienced in a normal flu season and yet we are about to dust off our
living wills.
The fact is, it is too late to worry if the current Influenza strain goes
full bloom into a Worldwide Pandemic. I had some really good feedback on my
latest article on the 2010 Pandemic (that has yet to
happen).
What I hope we will do is develop a third gear...an overdrive if you will,
that will take us into the future. Reinvigorate the National Disaster
Medical System...and some big time reinvigorating it will take. Lets develop
REAL plans to take care of REAL casualties. Lets do the hard work to develop
supply and equipment lists of all classes of materials, including packaged
disaster hospitals, needed for real people needing professional medical care
and sheltering and lets ask HHS or DHS to purchase and manage these critical
assets as Federal reserve Inventories.
Lets look at the 15 Federal Planning Scenarios and plan for the scenarios
which will most likely occur for our jurisdictions. Lets build packaged
disaster hospitals which are supplied and equipped with 60 days of supply
(DOS) without resupply. Lets really enhance our Medical Reserve Corps by
contacting every retired nurse and every certified nursing assistant,
physician, laboratory and radiology technicians, respiratory and physical
therapists and lets not forget the retired support staff. Lets also recruit
Psychiatrics, Psychologists and independent practice nurses. Lets link-up to
our communities and develop a real disaster-ready community response. Lets
ask the Federal Government do build Federal Reserve Inventories of food,
water, medical supplies, equipment and pharmaceuticals..to name just a few (FRIs).
After all, we already have the model in the Strategic Petroleum Reserve.
If we can muster the "Will," "Good Stewardship" and the funding to increase
our Readiness posture, we can take the first few steps that lead us to "Full
Readiness." We can begin saving hundreds of thousands of lives during the
next man-made or natural disaster.
Lets all insert that extra gear into our two speed culture. Let' see how it
feels to know that we did all that could have been done in preparing our
Country for the really big next one. That gear is known as the Readiness
gear. Start shifting!
Interim Lessons Learned - After Action Report on the 2010 Influenza Pandemic
[Jan 27 2009]
This is an interim “After
Action” report on a disaster. What separates it from other reports is that
this Lessons Learned report can be studied before the event actually
takes place. There may be time for Congressional Commissions to not only
assign blame for a lack of Readiness after the fact (as they tend to do),
but perhaps appoint personnel to the appropriate agencies capable of
learning these lessons and putting real systems in place before the
Pandemic. It is the hope of this writer that instead of simply assigning
blame and writing reports (as most After Action review committees do), the
Congress might actually proactively write language into laws that demands
operational systems and not just the kind of information papers that
currently serve as “readiness.”
Public Health Preparedness was very poor. The Department of Health
and Human Services (HHS) underestimated the Pandemic’s impact on the
American People in its initial estimate that approximately 92 Million
Americans would become ill and that approximately 45 Million Americans would
require some level of definitive healthcare, such as in a hospital. While
this Lessons Learned report only covers the first wave of the Pandemic, it
is clear that even more Americans will be impacted before the last wave of
the Pandemic travels across America. HHS was proactive in funding a number
of Public Health and Healthcare grant programs targeting syndromic
surveillance and Public Health laboratory capabilities. The syndromic
surveillance systems, while not perfect, provided advance detection of the
novel strain of Influenza almost immediately. However, the American people
already knew from news coverage, that the Pandemic was underway before the
first cases were detected in the United States. Some lessons learned from a
Public Health Preparedness prospective follow. Importantly however, most
States did not share Pandemic Preparedness grant funds with hospitals and
the “health care” infrastructure, opting to keep the Pandemic funds in the
Public Health sector. At the same time, States did not bolster the hands-on
care capabilities of the Public Health function, believing hands-on care was
the “responsibility” of the Private Sector Healthcare System.
Early detection was not enough. While early detection and timely
information to the public was laudable, there were virtually no actions
taken to treat the projected 92 million sick Americans. The Public Health
position was that public information, primers, and brochures fulfilled their
responsibility to alert Americans about a coming Public Health catastrophe.
Since no leaders in HHS, CDC or for that matter anywhere in the Public
Health Community were alive during the 1918 Pandemic, there was no way for
Public Health personnel to know how to care for the sick and dying. There
had also been no inclination on the part of Public Health officials to learn
how Public Health could expand healthcare services to augment the Healthcare
Industry. Thus, there was no “Plan B” in the Public Health system to
actually provide healthcare services to persons requiring definitive care if
the healthcare industry was unable to care for influenza patients. There was
no perceived need to provide additional resources for Private Sector
healthcare, since the American Healthcare Industry has the total
responsibility for providing actual healthcare services. In other words
Pandemic-related healthcare was a Private Sector matter, with Public Health
providing guidance only.
The CDC issued a timely Public Health Alert that a novel strain of Bird Flu
had mutated to the point of human to human transmission, at about the time
where the Pandemic was confirmed in Southeast Asia. Almost immediately,
Americans began checking their stocks of prescription medications as well
over-the-counter cold and flu products. As a result, before the first case
of the new Influenza was diagnosed in America, there was a Nationwide
shortage of virtually all prescription medications as well as
over-the-counter medications. What was not predicted by HHS or CDC was the
societal impact brought on by announcing the pending first wave of the
Pandemic. The unintentional consequence of the Public Health alert
announcement was an almost immediate failure of the pharmaceutical, medical,
food, fuel and retail supply chains. Since raw materials for many American
manufactured items are imported from outside the USA, all of these critical
supply chains will remain sporadic for approximately 3 years post-Pandemic.
In the meantime, those supplies which can be purchased will be in very short
supply. Federal officials warn that sporadic violence will continue
occurring as limited supplies arrive at retail outlets such as supermarkets,
drug stores, gas stations, and retailers everywhere.
The American Healthcare Industry was unprepared. The American
Healthcare Industry was totally unprepared to manage even a small percentage
of the affected population. The HHS, the American Medical Association, the
American Nurses Association, the American Hospital Association and virtually
every other known Healthcare Membership Association in America had warned
that the American Healthcare Industry was already in a crisis even without
any additional stress on the system. However, no Federal agency,
organization or association was empowered to do anything about the normal
operating crisis, let alone resourcing the Healthcare Industry to
effectively manage a major terrorist attack or the Public Health catastrophe
which is fully underway now. As a result most of the Healthcare Industry has
collapsed under the strain of this first Influenza wave. Since there were no
serious plans to drastically expand the Public Health Service to provide
“hands-on” health care, most Americans were left to care for themselves and
their loved ones. A simultaneous exhaustion of healthcare staff, the
healthcare supply chain and overcrowded hospitals, caused a collapse of the
entire American Healthcare Infrastructure.
The American Healthcare Industry collapse was due to a lack of elasticity
to expand for spikes in demand for a surge in admissions. While numerous
studies had confirmed that all study parameters were accurate and that all
models were valid, not all external factors were taken into consideration.
It seems no Federal agency had predicted a collapse of the American
Healthcare Industry under the stress of an Influenza Pandemic. Thus, due
to extreme shortages in facilities, healthcare providers, beds, medical
equipment, supplies and financial resources, American Healthcare collapsed
almost immediately during the early days of the Pandemic. It is anticipated
that the American Healthcare Industry will be rebuilt as a National
Healthcare System with some Private Healthcare entities providing elective
procedures. In any event, it will likely take between 10 to 15 years for
American Healthcare to achieve Pre-Pandemic operational capabilities. During
this time, religious organizations and charitable non-governmental
organizations will provide the bulk of the healthcare available in America.
Factors bearing on the American Healthcare Industry collapse.
1. Lack of Healthcare facilities: During the 1960’s the Federal
Government had approximately 1900 Packaged Disaster Hospitals. Each of these
hospitals had 250 beds, an X-Ray room and three operating rooms. Thus, as
far back as the 1960s, America had a total of 475,000 beds, 1900 radiology
suites and 5,700 operating rooms. All of these assets came totally outfitted
with equipment and sufficient supplies to remain self sufficient for 30
days. While there were a number of States that used Federal grant dollars to
purchase tent hospitals and other smaller care centers on rolling stock,
such as 18-wheelers, none of these care solutions were logistically
supportable or staffed for continuous operation.
2. Lack of healthcare beds. The Strategic National Stockpile had
stockpiled approximately 20,000 cots instead of beds. These cots were
unsuited to providing patient care in any facility and thus, were used only
for comfort care in patients’ last hours. These cots could not be reused,
since there were no decontamination instructions or equipment capable of
decontamination. These cots became single-use assets and were used up almost
immediately.
3. Lack of caregivers: While there were predictions of an extreme
shortage of caregivers, due to the shear numbers of sick Americans, no
Federal planning agency placed an actual number on how many skilled and
semi-skilled healthcare providers would be needed. As the first wave of the
2010 Pandemic swept across America, the requirement for additional
registered nurses (RNs), respiratory therapists, licensed practice nurses (LPN),
physicians, medical helpers and support staff rose to 10 million. While the
Medical reserve Corps had approximately 200,000 volunteers, many could not
respond due to obligations caring for their families or caring for
themselves. The end result was that religious congregations, the Red Cross,
Salvation Army and other voluntary organizations were and are currently the
only entities providing any meaningful care in the United States today.
4. Lack of Healthcare financial assets: Financial pressures on the
American Health Industry have been immense since the mid-80s. Government
reimbursements for Medicare and Medicaid have been tightening consistently
since at least 1985. Simultaneously, “Managed Care”, by way of the
healthcare insurance industry, had concentrated on driving healthcare costs
out of the system. Thus, both the Federal government and the healthcare
insurance industry drove down operational healthcare capabilities to a point
where a single, albeit catastrophic insult to the Healthcare Industry was
sufficient to cause its collapse.
5. Federal infusion of dollars made little difference. Similar to
America’s Financial System near collapse in the fall of 2008, by the time
that Congress recognized the American Healthcare Infrastructure was as
shallow as it was, it was too late to turn things around. In the Financial
System crisis, huge injections of Federal dollars propped up most major
financial institutions.
Unlike the Financial Crisis, injections of federal dollars made no
difference at all, since there was little product available worldwide. Once
the Pandemic was recognized, countries like China, America’s largest cotton
trading partner for surgical masks, surgical gowns, and patient apparel, had
stopped the flow of raw materials outside of their country. Similarly, other
countries that previously were our major trading partners for both raw
materials or for manufactured medical products, had shut down exports to
America in order to sustain their own populations.
While DHS, HHS and private organizations all understood that America was
operating in a “Just in Time” supply and equipment environment, Federal
agencies took no actions to build National Medical Reserves, as they had
with the Strategic National Petroleum Reserve in preparation for
interruptions in the oil markets. The global nature of supply chains for
food, medical supplies and equipment, and raw materials acquisition, while
the ultimate in efficiency, turned out to be useless in any unexpected surge
in demand. While Federal agencies well understood the “Just-In-Time” supply
paradigm, nothing substantial was done to eliminate or mitigate the impact
on America’s multiple critical supply chains, or the catastrophic
unemployment consequences the manufacturing, processing and distribution
industries faced when raw materials from overseas dried up.
6. Law Enforcement and Societal Norms. During the first several weeks
of the crisis, there was widespread looting and vandalizing of supermarkets,
drug stores, farmers markets and virtually any marketplace where food,
pharmaceuticals, baby formula and other items deemed necessary to provide
sustenance or treat the symptoms of Influenza were thought to exist. There
were widespread home invasions where gangs in search of food and medicine
took whatever goods they found, and then took other items of value in hopes
of trading these items for food later. The Law Enforcement and Public Safety
communities were themselves degraded in the area of law enforcement, and
were essentially out manned and out gunned to protect the population. As
expected, persons with disabilities, and the young and old subsets of the
population were especially vulnerable to attack (already being more
vulnerable to the ravages of the Pandemic and lack of needed food, medicine
and shelter).
As larger and larger numbers of Americans were too sick or too weak to
defend themselves, society lapsed into a more stoic norm, where religious
congregations and other charitable organizations provided the only
meaningful comfort for the sick and dying. Federal and State agencies were
staffed with employees who either recovered or seemed to have a natural
immunity to the novel Influenza strain. The services of these agencies were
well intentioned but almost totally ineffective. Sanitation across all
affected segments of society was deplorable. Municipal services including
waste collection essentially halted. The mortuary affairs departments of
State and local governments were overwhelmed with the dead.
Once again, religious congregations and charitable organizations represented
the only real remaining societal structure, picking up bodies much the same
as they did during the 1918 Pandemic and placing the bodies in communal
graves. Grave registries were mainly paper documents, but efforts were taken
to achieve a rudimentary accounting for those buried by gravesite.
7. Impact on the financial system. The financial system in the United
States has been decimated by the 2010 Influenza Pandemic. Officials are
advising Americans to retain all financial instruments, pending a recovery
after the third wave of the Influenza Pandemic. It is felt that any idea of
retirement based on a 401K or other stock market based instruments are lost
for a generation or longer. Still, the United States is expected to make a
more rapid recovery at least in comparison to many other countries around
the World.
8. Conclusion: It appears that a cascade of failures of America’s
critical industries and societal infrastructure began with Healthcare and
Public Health functions and have expanded out to municipal services and
finally to the fabric of society throughout the United States during this
first wave of the 2010 Influenza Pandemic. The results are and will likely
continue to remain characterized as “catastrophic” throughout the coming
waves. Many of these failings could have been and were anticipated. Better
preparedness in advance may have mitigated much suffering now.
9. Lessons Learned.
A. Develop a serious and sober listing of all Federal, State and Local
products, services and utilities that will be degraded or destroyed in a
Pandemic and fortify those areas immediately.
B. Build Federal Inventories of life sustaining goods such as food,
pharmaceuticals, over-the-counter medicines, clothes, shoes, and special
needs products for persons with disabilities, the old and the very young.
C. Pay manufacturers and distributors to manage federal inventories in order
that the taxpayer’s investments in these commodities can be preserved
through stock-rotation and quality control measures.
D. Enhance all critical infrastructure including items not normally
associated with Infrastructure:
(1) Religious and charitable
organizations that will do much to bring America back to normalcy.
(2) Bandwidth for the increase
in communication requirements for any disaster
(3) Healthcare. Private Sector
or not, these are the bastions of America’s health in a disaster or Public
Health catastrophe. Build a Public-Private enduring relationship with
every American hospital, nursing home, medical center, specialty center,
community center etc., because in a disaster, they are all we have….and
federally fund disaster-related hospital expansion programs.
(4) Purchase a minimum 1,000
portable rigid or semi-rigid walled healthcare structures, 200 beds each,
with radiology and operating capability for long term use during any
disaster that destroys American communities healthcare infrastructure.
(5) Build a logistical support
system with civilian and military transportation assets sufficient to
re-supply every healthcare entity in America during disasters.
(6) Assign Public Health
Agencies a “hands-on care mission” for relieving the enormous stress
hospitals, nursing homes and medical centers will experience during a
pandemic. Provide funding not influenced by the “partisan dabbling” we have
seen in our past.
(7) Insist on a Good Steward mentality for Government agencies and federal,
state and local leaders at all levels of government. Rid ourselves of
Government power brokers and castle builders and replace those shallow souls
with Americans who seek the good of the People, well above any petty
self-interest.
Please let the process begin today!
Building and supporting a positive culture of preparedness
[Jan 5 2009]
I have been involved in community preparedness all of my adult life and have had the good fortune to work with some of the best folks in the Emergency Management field. When I read some of the conversations on this IAEM List, I thought I’d comment on the types of personal qualities that promote and foster a “Culture of Preparedness” in jurisdictions and communities. For readers who like the bottom line up front, I’ll provide it here.
If you are working for an elected official who is not committed, do whatever you can to help this person become a real Community Preparedness leader. It will not be easy to foster this change, but try to exhaust all possible strategies within your scope.
If you can’t help the elected official, it may be time to find a community whose elected official wants to be prepared and elected leaders who will support you. If you remain in a community and just go with the flow so to speak, you are truly a part of the problem.
Listed below are some traits that are absolutely necessary in Emergency Management leaders at all levels of government.
A Visionary: I think it was Walt Disney who said “If you can dream it, you can do it.” In our context, if the Emergency Manager does not have a clear vision of how his/her community must plan, train, test, learn and manage future disasters, he or she cannot lead their communities toward a Culture of Preparedness. The old mentality “we can all reach consensus and come together as involved stakeholders” sounds great and utopian but is a bunch of bunk. Someone needs to see the Big Picture, and have the requisite zeal for achieving the results of that Big Picture… and that person is the Emergency Manager at the local, state and federal level. True, the Emergency Manager can only be effective if the elected officials are truly committed to Preparedness, but the Emergency Manager is definitely the right person to articulate the vision of real community Preparedness.
A Leader: The National Response Framework (NRF) is useful in that it outlines very important concepts such as NIMS, an integrated Incident Command System where all stakeholders are a part of the total response. What the NRF is no good at providing is a no-nonsense “who does what for whom…and when” delineation of responsibilities. It seems that in America today, we don’t want to be demanding of others and we absolutely hate failure, so we engineer systems that can’t fail. Of course these “wiggle plans” can’t succeed either as we saw in recent disasters including hurricanes Katrina and Ike. New Orleans and Galveston Island are still living with limited or no Healthcare and Public Health infrastructure.
The Leader at the city and state levels of government needs to publish a clear and concise list of “measurable responsibilities” for the individual, local organizations (for-profit and non-profit), Non-Governmental Organizations, local governments and state governments. The plan needs to be clearly articulated using every possible media format and it must be signed by every stakeholder organization. We have seen all of the advertising on what we need to do to become “Digital TV Ready” on terrestrial, cable and satellite TV channels. Where are the 30 second spots on “what I need to do to become prepared” for the types of disasters listed in the jurisdiction’s Hazard Vulnerability Assessment (HVA)? Are we more concerned with getting “American Idol” than we are at getting prepared?.....apparently so.
When I start seeing public service announcements (or paid spots) on TV informing me of the types of events for which I need to prepare and what I need to do and have available in my home, I’ll know we are headed down the right path to Preparedness. Public Information is a mandatory part of developing a Culture of Preparedness.”
If you need to pay Risk Communicators to effectively send the message, pay them. If you need to pay radio and TV stations to run the ads, pay for them. If your elected officials will not support Community Preparedness, no matter your efforts to advance this, perhaps it is time to dust off your resume. There are many communities that with committed leadership truly want to become prepared…. find them.
A Good Steward: Every Emergency Manager in the United States is a “steward” of our tax dollars in the area of Emergency Management and Preparedness. I shudder when I hear Federal officials say the words “Use or it lose it” when applied to appropriated monies. If ever there was a verbal mandate for waste, fraud and abuse, this is it. No activities, projects or programs should be funded without clear plans, desired outcomes and measurements. Measure fearlessly! If you aren’t failing in some areas, your community is not discovering ways to do things better and recover sooner.
All available funding should support the Preparedness vision mentioned above and not personal wishes. The “Good Steward” buys Preparedness and not preference. There is no “what’s in this for me?” question in Good Stewardship. I happened upon the test for stewardship when I was in charge of medical war reserves in Europe. For just one item, (nerve gas antidote) I could either spend $10 Million on Mark1 Autoinjectors which were expiring (there is no normal use for Mark1 Autoinjectors and thus no stock rotation opportunity), or hope that the FDA would extend the shelf life on over a million units of expiring Autoinjectors. If I purchased new product and the FDA approved the shelf life extension, I’d have $10 Million in excess Mark1 kits…a very bad place to be when the General Accountability Office visits …and it will. On the other hand, if a war broke out and I elected not to replace the expiring Autoinjectors, hoping for that shelf life extension, I’d be in the position of issuing expired antidote Autoinjectors. I decided I’d rather explain to the GAO and to Congress my rational for replacing the antidote, than I would try to justify to parents and loved ones of Servicemen and woman why their loved ones had to use expired antidotes. I did the right thing and was prepared to defend my stewardship of taxpayer’s money. As it turned out, the 1991 Gulf War broke out. We had the required on hand assets of serviceable Mark1 kits and we had made the right decision.
A Teacher. As every teacher knows, helping others learn is a real challenge, but it definitely has its rewards. The Emergency Manager is the expert in all aspects of Emergency Management and that knowledge should be shared with all stakeholders and the next generation of emergency managers in the agency. It is hard work meeting with groups of elected officials, other agencies, elected officials, healthcare executives, public health officers, non-governmental organizations and civic groups. The fact is, we need the entire community’s participation and commitment in developing a Culture of Preparedness. On top of that, it takes stamina to keep the commitment to Preparedness alive and vibrant in the community. We all want to get “comfortable” in our daily lives and in our normal jobs. It is the Emergency Manager, who as the teacher and mentor keeps the Culture of Preparedness alive and young in our communities.
It’s a tough job and at times a thankless one. In that 1991Gulf War, I certainly was concerned that there would be casualties and fatalities on both sides. The one thing that I did not worry about was our ability to medically support our troops. I can’t even imagine the horror, shame and sadness I would have felt if I had made decisions based on the safe thing to do for me in the months and years leading up to the war. Emergency Managers will never feel good about a disaster that befalls their community. What can happen though is that each Emergency Manager as a visionary, a leader, a good steward and a teacher can attack future disasters knowing that he or she did the right thing and pulled out all the stops to assist their community achieve a real Culture of Preparedness.
Leadership and the culture of preparedness
[Jan 3 2009]
Pandemic planning and regulated medical waste
[Oct 24 2008]
It seems everywhere we look today; there is information on how we as a society can prepare for a new strain of avian influenza capable of ravishing our communities.
The fact that it will be a new (novel) strain of influenza
means that there is no immunity to the new virus in the
general population, or indeed on earth.
Mankind’s lack of immunity to the new virus is at the heart
of a Pandemic. Pandemics have occurred in the past and will
continue to occur in the future. It is estimated that up to
one third of all Americans may be infected during the
Pandemic and as many as 45 Million Americans will require
some level of definitive medical care.
This is especially bad news for hospitals, medical centers
and healthcare systems already
functioning at or near capacity.
In order to manage a Pandemic, many Public Health Officers
around the County have dusted off and updated quarantine
laws which are designed to cut the Pandemic’s lifeline to
new hosts (people) to infect.
If Public
Health Officers can significantly control access into and
out of their jurisdiction, it is hoped that the disease can
be encircled, isolated and contained within the quarantined
jurisdiction. In that way, the virus cannot perpetuate
itself as efficiently and as a result, it dies out.
While
Quarantine has been recognized for centuries as an effective
tool for controlling contagion, it has a number of dire
unintended consequences.
One of the
consequences is the accumulation of normal and
pandemic-associated untreated healthcare regulated medical
waste (RMW).
How are
hospitals that use “off-site” transportation and treatment
services for medical waste going to rid themselves of their
infectious waste?
The fact is,
“they have a problem.”
The last thing Public Health officials need are mountains of untreated medical waste piling up in hospital parking lots throughout their jurisdiction.
Most probably, the Environmental Protection Agency would
suspend “clean air regulations” and allow healthcare
organizations to resume incineration of RMW.
Of course the
issue here is that most hospital incinerators were
decommissioned and removed after passage of Clean Air Act of
1970 and the Resource Conservation and Recovery Act (RCRA)
of 1976. It became clear that there was no come-back likely
for onsite incineration. There is a solution to this problem
and it is “Back to the Future” in effect.
Since the
heydays of the incinerator, alternative “on-site RMW
treatment technology has advanced to the point where it is
the most socially-responsible, environmentally friendly and
cost effective method to treat medical waste at the
healthcare facility level.
Many
healthcare professionals believe that once their medical
waste is handed off to a transporter, the healthcare
organization is “off the liability hook.” Not so according
to RCRA.
Regulated
medical waste is the responsibility of the generator (in
this case the healthcare organization) from the “cradle to
the grave”, or in other words until the medical waste is
rendered safe.
Sometimes
necessity truly is the mother of invention. As Public Health
Officers continue to work on Pandemic Preparedness, many
will examine the possibility of using Federal Grant dollars
to enhance America’s Pandemic preparedness with on-site
medical waste treatment technology.
On-site RMW treatment technology reaps immediate benefits by reducing the amount of RMW being transported through American communities and across our roads and Interstate highways. It also protects healthcare workers and conserves valuable landfill resources.
It’s the right thing to do and the right time to do it.
Healthcare disaster preparedness and gap analysis - What it truly entails?
[Sep 8 2008]
With Hurricane Ike in the news, I thought I'd share an article I wrote some time ago on how healthcare organizations can perform a quality “gap analysis” to identify unmet requirements and then to work on narrowing the gap between what is required versus what is on-hand and available through local suppliers to build a robust and resilient healthcare organization. Also, since The Joint Commission (TJC) has significantly broadened and emphasized healthcare Emergency Management standards for 2009, this article may be timely for those preparing for TJC surveys.
Everywhere we look these days, there seems to be guidance suggesting that healthcare organizations should perform a complete “Gap Analysis” as part of their Emergency Management Program (EMP). What seems to be lacking, is a recommended process to perform the “Healthcare Gap Analysis.” This process is also relevant to Public Health Departments. The jurisdiction’s Emergency Manager’s participation and leadership in Gap Analysis is vital to this process.
There are four major components to a thorough Gap Analysis: (1) Identification of planning scenarios along with the number of anticipated casualties for each planning scenario; (2) Requirements development; (3) A listing of current resources and capabilities; and (4) Identification and forwarding to the next higher support agency, the gap between current resources and capabilities and the total requirements needed for each planning scenario. The following is an attempt to clarify the various components of a complete Gap Analysis process.
1. The Planning Scenarios and the estimated number of casualties (live patients). What types of emergencies are likely to befall a jurisdiction and how many casualties will likely be generated by each planning scenario? To get to these data, healthcare planners must consult with the jurisdiction’s emergency management agency. The jurisdiction’s Director of the Emergency Management Agency (EMA) performs Hazard Vulnerability Assessments (HVA) for the entire community. Based on these HVAs, healthcare planners can obtain a number of planning scenarios which the jurisdiction could reasonably face. While healthcare planners may consider many planning scenarios, for this discussion we will base the Gap Analysis on the top 3 planning scenarios provided by the EMA. For each planning scenario, the healthcare planner must also obtain estimates of the number of patients that will be generated. The EMA can often estimate the numbers of casualties (patients) and fatalities (dead), as well as the categories of injuries (such as burns, blunt force trauma and blast) for each planning scenario based on past disasters - such as the London bombings or the Tokyo subway Saran attack. The local or state Public Health Officer is the source for estimating the numbers of infected patients generated by events such as a SARS outbreak or a Pandemic Influenza. HHS and Public Health sources such as the Centers for Disease Control and Prevention may also provide estimated numbers of infected persons based on a jurisdiction’s population and may also offer advice as to the likely percentages of patients who will require hospitalization. The Agency for Healthcare Research and Quality (AHRQ) also has a variety of very helpful tools and documents to estimate casualties from a number of disaster events.
2. Requirements Development. Another way of phrasing this component is: “what resources will be needed to treat the numbers and categories of patients injured or infected as a result of each of the top 3 planning scenarios?” The requirements component of Gap Analysis is the process where healthcare organizations identify every resource that will be required to effectively treat the estimated numbers and categories of patients resulting from scenarios identified in the community HVA. Hospital requirements in facilities include: beds, staff, medical supplies and equipment (such as ventilators, specialty beds and surgical equipment), transportation, food, water, generators/emergency power capacity, fuel, medical waste treatment equipment or service, or any other resource required to treat the numbers of estimated casualties for each of the top 3 planning scenarios. The requirements or “needs” of the organization must not be influenced by what resources the hospital has on hand or can readily purchase from its suppliers. Facility “requirements” and “available assets” must remain separate. The reason why the requirements component must be separated from available resources will be discussed in items #3 and #4, below. While the requirements development portion of a Gap Analysis is not a difficult process, it is tedious and time consuming. Perhaps that is why the requirements process is often the most poorly defined component of the Gap Analysis.
3. Current Resources and Capabilities. This component of the Gap Analysis process depicts the entirety of the resources the healthcare organization has at its disposal against the number and categories of patients it needs to treat. Many healthcare planners feel that they must somehow obtain the additional resources needed to manage a given scenario. The reality is that the National Response Framework (NRF) anticipated that requirements will far exceed local and even state/territory resources. The Emergency Support Function (ESF) organization at the Federal level responsible for providing Public Health and Medical Services sustainment support is the Department of Health and Human Services (HHS) as the ESF-8 agency. HHS is tasked to provide the difference between city and state/territory available resources and capabilities and the total requirements and capabilities needed to medically manage large scale events. It is therefore imperative that local and state/territorial resources and current capabilities and the “Gap that exists between “Requirements and On-Hand assets” be expressed accurately. Only then can the HHS (and other Emergency Support Functions) properly plan, program and budget for the “Gap” that exists in jurisdictions across America.
4. The Gap Analysis and what to do with it. The “resource and capability gaps” for each planning scenario is the difference between available resources and capabilities and the total requirements. The National Response Framework requires that local healthcare organizations pass on requirements exceeding available resources to the local Emergency Management Agency (EMA). The unmet requirements which cannot be met at the local jurisdictional level must then be forwarded to the state/territory or Tribe EMA. Finally, unmet state/territory/Tribe unmet requirements for resources and capabilities will be forwarded up the chain to the Federal agency responsible for providing the individual Emergency Support Functions (ESF). In the case of Public Health and Medical Services, the Federal support function is ESF-8, and is provided by the Department of Health and Human Services (HHS) and the various support agencies.
By well-defined Gap Analyses from jurisdictions across America, HHS can then analyze, plan, program, budget, procure and pre-position additional resources and capabilities needed to close Gaps and sustain and fortify America’s Public Health agencies and the private healthcare industry during future emergencies and disasters requiring Federal support.
If the Gap Analyses at the hospital and health system are properly depicted and routed through the local and state Emergency Management Agencies, Federal Emergency Support Functional agencies can program for the entire array of “unmet requirements” including mobile medical units, as well as a full complement of staffing, medical and non-medical supplies, equipment and services required to support state/territory and local governments during future disasters and public health emergencies. For example, if the Gap Analysis discovers a hospital’s back-up power generator is insufficient for “long run power generation” (sometimes called an intermittent short duration back up generator), perhaps in the earliest stages of a disaster, the State EMA could immediately deploy long-run power production back-up generators to those hospitals. An even better solution would be for Emergency Managers to proactively work these challenges with healthcare executives and share DHS/FEMA grant dollars to close back-up power capability gaps. Compared to evacuating, tracking patients to healthcare organizations outside the affected communities, the proper power production generator, connected to all vital hospital utilities (including HVAC) is a real bargain.
It is imperative that healthcare, public health and jurisdictional emergency managers work extraordinarily closely in identification of all gaps in resources and capabilities and forward the appropriate unmet requirement gaps up the NRF support chain in order to ensure the healthcare and public health needs of communities are met during future man-made and natural disasters. If quality Gap Analyses are conducted and acted upon proactively, we may see healthcare organizations and public health departments performing brilliantly in future disasters, saving and protecting the lives of those in the communities these organizations serve.
Surge Capacity...and the American healthcare system's [in]ability to respond to the next catastrophe
[June 28 08]
I wish we would stop studying
our healthcare industry's inability to respond adequately to
a large scale disaster. It's really quite simple....the
healthcare industry has been in crisis for over 20 years and
many (if not most) ER's are on "Divert Status" during
weekends and normal spikes in demand for health care
services. The American Healthcare Industry cannot respond
effectively and won't be able to respond effectively to any
Large-Scale disaster. The reason: The American Healthcare
Industry is not funded to surge to manage large-scale
disasters. Man, was that a thrifty Readiness Assessment.
I'm even tired of hearing myself say this in article after
article. Sure, healthcare entities can surge for short
duration, medium intensity events using the integrated
healthcare approach outlined in Federal grant guidelines.
Healthcare organizations can make the most of integrating
healthcare systems locally and even regionally. But still,
an integrated approach will still not cope with the numbers
of patients associated with a Pandemic or the huge numbers
of casualties resulting from a nuclear attack-and never will
be capable of this level of healthcare response. Just like
we pool our tax money together to form an Armed Force
instead of local militias, so too must we fund a National
Health and Medical entity to deal with National catastrophes
like hurricane Katrina, a nuclear attack or a Pandemic. I
know we shudder to think of the Federal Government managing
anything, but we must do this and hold the Federal agency
fully accountable for Full National Readiness.
We need the Federal Government to respond as they did back
when we actually believed we could be attacked by the Soviet
Union. The Federal program was called the Civil Defense
program. In the '60s America had 1900 "Packaged Disaster
Hospitals" and each one of these mobile assets had 250 beds
with X-ray and surgical capabilities. These died of old age,
expiration of supplies and neglect. This was due to funding
cut offs, when somebody probably decided a full-out nuclear
war would wipe us all out...so why prepare?
I know this sounds very antiquated, but these disaster
hospitals would have served America well if we hadn't
abandoned the concept in the '70s. If we had these disaster
hospitals and their staffing and logistical support systems
in place today we would be in very decent shape for the 15
Federal Scenarios we talk about today. However, even if we
had a network of sustainable hospitals, we would still need
an air, ground and rail system to move casualties/patients
to areas of America where specialty care was available. This
is where the National Disaster Medical System transportation
element would shine.
I believe our Transportation Industry would work with the
Feds IF the federal government bought airframes, ambulance
helicopters, ambulance buses, rail cars (there isn't any
real excess capacity out there) and built a National ground,
rail and air Evacuation system. The Federal leadership is
also going to have to bolster other supply chain systems
like our food and water supplies, over-the-counter drug
inventories etc.
Wouldn't it be great if the National Public Health
Information Network (PHIN) was linked to the food supply
chain networks? If we had the capability, CDC could link
syndromic surveillance peaks from the jurisdiction suffering
illness spikes, back through each element of the food supply
chain. Jeeze this is great! We might be able to do the same
thing for medical products to quickly track down product
tampering. Maybe these types of initiatives would be
identified by Congressional committees as "Successes in
Imagination."
The Medical Reserve Corps and ESAR-VHP programs are working
well but need massive expansion. The National Disaster
Medical System must be re-invigorated well beyond its
current capabilities. Every single retired physician, nurse
(all specialties), respiratory therapist, optometrist,
psychologist, etc. must be aggressively recruited to join
the National Disaster Medical System (NDMS). The NDMS must
be returned to its highest state of readiness and then still
further bolstered to medically manage a Pandemic and/or a
nuclear attack or other large-scale man-made or natural
disaster.
The Public Health Service Commissioned Corps and civilian
employee ranks must be seriously bolstered with personnel,
facilities, a Federal Reserve Inventory (FRI) of Pandemic
and Nuclear related supplies, equipment and service
contracts to supercharge the NDMS during a Pandemic or a
nuclear attack. Federal Reserve Inventories are needed (Just
like the National Petroleum Reserve) for very large spikes
in demand for medical supplies & equipment, food, water,
special needs supplies etc. We all live in a World Economy
and a Just-In-Time healthcare and food supply chain. I'd
hate to see over-the-counter medicine on sale at eBay during
a Pandemic, but we will.
How much will this all cost? About the cost of one
Nimitz-Class aircraft carrier $4.2-$5.0 Billion. I am all
for a powerful Navy, so I'd be the last to criticize the US
Navy's investment in any of the fleet craft. We need to
adopt the budgetary processes of the DOD.
There is one very big difference between the Armed Forces
and Public Health community. The DOD gets an approved
Mission from Congress, then outlines in budgetary documents
all Requirements it needs and the costs of each line item to
perform the mission. The DOD chops on it, so does the
President and Congress; it's their jobs. The job of the DOD
is to lay out the items and the costs.
In the case of Healthcare and
Public Health Readiness, it seems Congress arbitrarily sends
an allocation to HHS and says "Do things with this money." I
was an HHS/HRSA employee and I could never understand why we
didn't send up to Congress a Requirements Statement along
with the line item of each requirement. I know the people
are great, but I still don't get it.
For the life of me, I can't figure out why HHS doesn't take
the DOD approach. Once again I like HHS very much and I know
some extraordinary and devoted people at HHS and CDC...it's
not that I have an axe to grind; I don't. However, every
time I hear the words (paraphrase) "We are not at full
Readiness, but we are more prepared than we were" I get
mildly ill and sometimes I kick dirt. Simply put, that's not
going to cut it anymore.
The American people deserve to know the line items and the
Price Tag of what DHS and HHS needs in order to reach 100%
readiness to care for Americans during a Pandemic or a large
scale terrorist attack like a nuclear detonation. It's not
cheap, but lets give Congress the opportunity to vote on
appropriations ...it's their job for crying out loud. And
I'm crying out loud that it may be too late for the next big
event.
Healthcare and public health disaster readiness made easy
[June 9 2008]
I recently took a breather from Healthcare
Readiness and returned to Healthcare Administration to recharge my spirit
and to get back to doing real healthcare operations. I was really burned out
from reading and writing scholarly articles on Readiness and wondering when,
or if indeed if I’d ever get to actually do things again. OK, my articles
weren’t scholarly at all, but I tried. Being a high energy person who loves
serving people, my healthcare hiatus was just what the doctor ordered. In my
case, the doctor was my wife and she also ordered me home…I can’t understand
why. One of the things I took away from my recent “on-the ground” healthcare
experience was just how demanding Healthcare leadership is in an environment
of dwindling resources. Now that I’m back, I thought I’d try to write an
article on how Emergency Managers and Healthcare leaders can work together
to offer their communities the best chance of surviving future disasters.
1. Share the Community Hazard Vulnerability Assessment. Many healthcare
planners are not in sync with their community Emergency Managers regarding
the likely disasters the EM is planning for; and the categories and
estimated numbers of patients healthcare organizations should plan to
receive for each planning scenario.
2. Jointly develop the requirements for staff, materials and service
contracts needed for each scenario. It would be counterproductive for the
Emergency Manager to plan for a nuclear detonation scenario and keep
Healthcare leaders in the dark about the types and numbers of casualties
such an event will likely produce. Some questions for consideration:
• How many extra medical staff will be needed to manage the healthcare
response?
• How can Emergency Managers help hospitals in communicating with,
transporting and providing security for health workers arriving from state
networks for Volunteer Health Professionals (ESAR-VHP) and state and local
chapters of the Medical Reserve Corps (MRC)?
• How will hospital suppliers re-deploy supplies from one region of the
country to the disaster location?
• What supplies and equipment (plus quantities for each item) will be needed
to respond effectively to each planning scenario?
• How will hospitals order and receive Federal equipment and supplies and
what supplies and equipment are available?
• How can community volunteers help with and augment security, escort and a
host of other required hospital functions?
• How will the hospital acquire oxygen, water (potable and washing/chiller
water), food and back-up generator fuel throughout a disaster?
• How will medically stabilized patients be transferred (patient regulating
and tracking office) and transported to specialty centers outside the
disaster location?
• How will loved ones receive healthcare information relating to the status
of their affected family members?
• How will hospitals communicate with the EOC/alternate EOC?
• How can the Emergency Manager help Home Health agencies/organizations get
power back-up equipment, supplies and food to homebound persons?
• How can healthcare organizations cooperate fully with other healthcare
organizations/systems and the Emergency Management community during
exercises and gain from past failures and lessons learned?
• How can the Emergency Manager help fortify the hospital/medical
center/nursing home so that evacuation becomes the last resort that it must
become?
3. Facilitate the cooperation between hospitals and indeed competing
healthcare systems. Why? In any widespread disaster it is in the best
interest of competitors to work together so that they can both get back up
and running after the disaster.
4. Assist healthcare organizations in planning for the care of vulnerable
persons during and after a disaster?
5. Help with healthcare recovery efforts, for example temporary & long term
shelters, access to care, sanitation, water & waste systems, oxygen, food &
special feeding systems and back-up power for all shelters, especially
special needs shelters.
6. Help educate Public Health officials that in a pandemic or other public
health emergency, the Public Health Officer will be the responsible Public
Official for protecting public health and providing care for the
community….. It’s called Community Surge. Healthcare organizations aren’t
designed or resourced for Public Health catastrophes. As of this writing,
many Public Health Officers throughout America are not accepting
responsibility for caring for the community during the coming pandemic.
Since the Emergency Manager is where the buck stops, it’s only fair that you
task the Public Health Officer with Community Surge responsibility….but wear
PPE.
7. Finally, I said this was easy didn’t I. Actually I was fibbing, it’s not
all that easy but it can be done as long and we care about each other; share
resources, information, subject matter expertise, and good old elbow grease.
Emergency Managers realize two important things. First, the communication,
transportation, sheltering, provisioning sustaining and caring for the
community will all have to be accomplished either before or during a
disaster. Second, healthcare leaders don’t work Readiness issues for a
living and many Public Health officials haven’t yet accepted that their part
goes well beyond syndromic surveillance and education in a public health
catastrophe.
The fact is many healthcare executives haven’t faced the reality that the
very existence of their organization may very well depend on comprehensive
Disaster Readiness planning and coordination with other healthcare
organizations as well as their emergency management community. Likewise, the
American public health enterprise hasn’t universally accepted the mission of
providing care for Americans during a public health catastrophe like a
pandemic or a large scale biological weapon attack. It seems to me that as a
public official, the Emergency Manager is the best resource we have to get
the Healthcare Industry and Public Health Community on the same page. As
such, you represent the best chance American jurisdictions have in surviving
future disasters. It may not be all that easy, but it’s true.
Adapting a Battlefield Medicine System to Civilian Mass Casualty Events
[Jan 7 2008]
As part of the disaster preparedness planning process, many emergency managers, especially in large metropolitan areas, are facing the realities of a possible London or Madrid-style mass casualty scenario. Even more disturbing, emergency managers in financial and political centers which are likely considered “high-value” targets by terrorists are facing the prospect of thousands or tens of thousands of casualties and evacuees associated with a nuclear attack. Overwhelming numbers of casualties in a truly catastrophic event can be managed by looking at healthcare models affectively used on the battlefield.
This writer was fortunate enough to be a part of a 1980 US Air Force initiative which adopted many of the lessons learned by the Israeli Defense Forces in battlefield medicine, particularly during the Yom Kippur war in 1973. This system, called the 4-Echelon Battle Casualty Management System, can now be adopted by emergency planners and managers for managing mass casualty scenarios in civilian settings.
Introduction to the 4-Echelon Mass Casualty Management System.
Battlefield casualty management experience has resulted in advanced and effective rescue, resuscitation, stabilization, definitive treatment and rehabilitation of soldiers ever since World War II. The use of the helicopter as an air ambulance greatly improved the survival rates of soldiers wounded in combat in Korea and Vietnam and in all conflicts since. Many trauma procedures develop in combat medicine have been applied with great success to our civilian trauma systems. With the ever-present threat of terrorist attacks using biological, chemical, radiological/nuclear and explosive agents or devices, the time may be right for jurisdictions and their civilian healthcare systems to implement a combat proven system for mass casualties called the 4-Echelon Mass Casualty Management System.
For more than 10 years, Public Health agencies at all levels of government have been ramping up capabilities for early detection and responses to biological warfare agents and disease outbreaks. Public Health planners have also developed strategies for providing rapid post exposure medications and vaccinations to millions of people affected by these man-made and naturally occurring events. The time is right to forge strong relationships between the Emergency Management community, Public Health agencies and Private Sector healthcare organizations in planning for large scale disaster or emergency events..
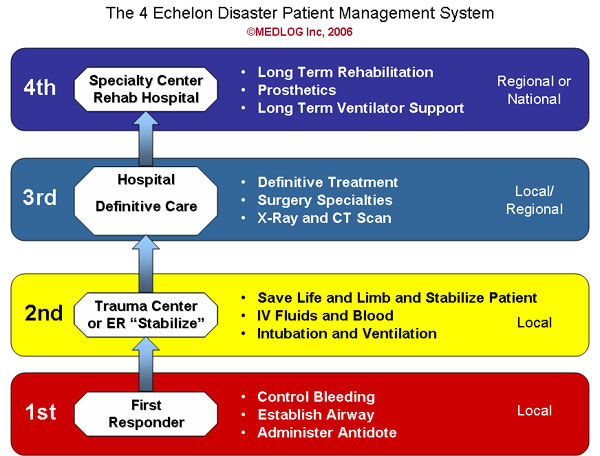
What is the 4-Echelon Mass Casualty Management System? The 4-Echelon Mass Casualty Management System is a highly effective and efficient system of managing very large numbers of casualties throughout a disaster and until local healthcare organizations recover and can resume normal operations.
The 1st Echelon of care is provided by first responders and consists of immediate lifesaving procedures and the rapid transport of the living to a 2nd Echelon facility.
A 2nd Echelon facility may be a trauma center or an emergency department. The 2nd Echelon is essential in making the most of the patient’s “Golden Hour.” By providing immediate care and by dramatically increasing the casualty throughput to 3rd and 4th Echelons, the 2nd Echelon care providers prevent or reduce the patient gridlock associated with a disaster and thus, optimize the saving of lives. 2nd Echelon care is designed only to save lives and stabilize patients and not to provide definitive care. Employing the latest advances in trauma care, 2nd Echelon care includes procedures for saving life and limb and stabilizing patients. Typically at the 2nd Echelon, providers ventilate patients if necessary, control bleeding, infuse blood products and expanders and amputate limbs as required. Once stabilized, patients are quickly transported to the 3rd Echelon of care for definitive treatment.
The 3rd Echelon of disaster healthcare is typically a hospital or medical center away from the immediate disaster location. In the early stages of a disaster, a hospital or medical center may provide both 2-E and 3-E care. It is likely that a hospital’s 3-E capacity will almost immediately be reached and the facility will revert to 2-E care only. 3rd Echelon facilities may be within a jurisdiction or may include hospitals in several jurisdictions or even national regions, depending on the number of casualties and the care requirements. Definitive care is provided at all 3rd Echelon facilities, but specialized care such as burn centers may also be provided in a 3rd Echelon facility. This includes a full complement of surgery specialties, diagnostics and follow-on care for about 7 days. Patients who cannot be discharged within a week are normally candidates for 4th Echelon care.
The 4th Echelon may include specialty centers or rehabilitation hospitals capable of providing long term ventilation care, psychiatric care, burn or wound care and rehabilitation or specialization in physical therapy or orthopedic care including providing prosthetic devices and associated therapies.
Depending on the location and scope of the disaster, a particular hospital may function as a 2nd, 3rd and 4th Echelon facility. When close to the disaster location, a hospital may have to function only as a 2nd Echelon facility, transporting all stabilized patients to 3rd and 4th Echelon facilities further away from the disaster location. By so doing, the hospital serving as a 2nd Echelon hospital may be able to accept more patients in need of stabilization than it could as a multiple-Echelon facility. In another disaster scenario further away, this same hospital could be functioning as a 3rd or 4th Echelon facility, providing definitive and/or specialty care to stabilized patients.
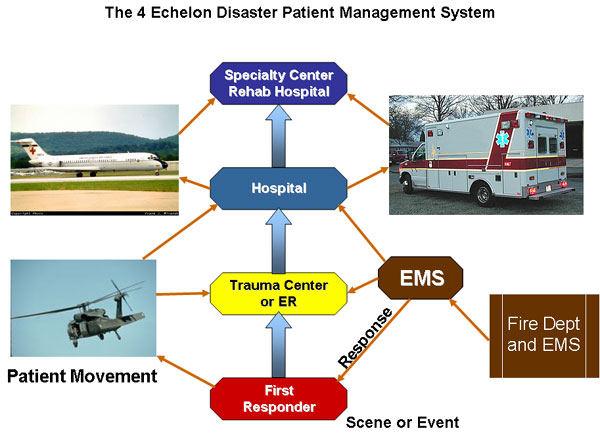
What is the role of Healthcare Organizations as part of a 4-Echelon Mass Casualty Management System? Most medical centers and many hospitals operate as full 4-Echelon capabilities during normal everyday operations. During a disaster, Healthcare organizations will periodically self-declare their capabilities to the Emergency Operations Center (EOC) in terms of the Echelon of care they can provide in a fluid environment. Depending on the size and scope of a Mass Casualty event, a hospital may eliminate the 4th-Echelon immediately and declare itself as 2nd and 3rd Echelon capable to the medical representative in the Emergency Operations Center. At that point, the EMA would reach out to adjacent jurisdictions to activate their EOC (s) and to provide a list of healthcare organizations capable of providing 4th Echelon care. At some point in disaster operations, an individual healthcare facility may declare itself limited to 2nd Echelon care only, thus requiring outside healthcare support at both 3rd and 4th Echelons. In fact, in some circumstances, a healthcare organization may reach full capacity and be incapable of accepting any additional patients. In other cases healthcare organizations may be damaged in the disaster and may need to report to the EOC that all patients must be evacuated and transported to healthcare organizations outside the affected area. In any case, healthcare organizations must be able to efficiently communicate their capabilities with the jurisdiction’s EOC throughout the disaster.
How can 4-E work in a competitive Healthcare Marketplace? A traditional model of disaster healthcare seems to dictate that healthcare organizations provide the full continuum of care to all patients presenting for care. Competition would seem to dictate that hospitals or medical centers expand (surge) their services until their individual capacity and capabilities are reached. Why then would hospitals want to self-declare themselves as a 2nd Echelon facility and request rapid transport of stabilized patients to healthcare organizations outside of their service area? The answer lies in continuity of operations. Hospitals in the affected area need to recover and resume normal healthcare services as soon as possible after a disaster. By serving as a 2nd Echelon facility and rapidly transferring patients to 3rd and 4th Echelon facilities outside the affected area, hospitals and medical centers in the affected area can conserve staffing and material resources and thus, can more rapidly recover after the disaster event.
This definitely requires a paradigm shift, but experience shows that after a disaster, healthcare providers need decompression time. If the staff is exhausted, who will provide healthcare services immediately following a disaster? Likewise, medical supplies are consumed at an enormous rate during a disaster. Equipment used during a disaster needs to be disinfected and inspected prior to being returned to normal service. If the support services personnel are exhausted, who is going to disinfect hospital areas and the equipment and how long will the hospital be closed after a disaster? Heart attacks and strokes will still occur, babies will be born and the population in general will need care immediately after a disaster.
Finally but importantly, disaster operations can and do strain healthcare financial resources to the breaking point. The last thing that any community needs after a disaster is a number of bankrupt hospitals or medical centers. Civilian healthcare organizations cannot issue continuing resolutions in order to make payroll or pay suppliers during and after a disaster. Federal and State payers as well as private insurance companies must develop and publish simplified health care claim procedures for use during declared emergencies. These simplified claim procedures will sustain healthcare organizations and their services during and after a disaster and can help ensure that healthcare services are available after the disaster. Perhaps, simplified financial procedures can be tied to services rendered at each Echelon of care.
Adopting the 4-Echelon Mass Casualty Management System. The first step is the adoption of the 4-Echelon Mass Casualty Management System by a state or territory EMA and the Healthcare organizations within the jurisdiction. Once proven in a single state, the 4-Echelon System may be adopted throughout a federal region or multiple regions. In time, the 4-Echelon System can be adopted Nationwide. The 4-Echelon System will fit seamlessly into the National Disaster Medical System (NDMS), since NDMS healthcare facilities were the planned 4th Echelon of care for service members returning from either the European or Pacific theaters of operations, had the Cold War turned hot. Although the 4-Echelon System never needed to be fully implemented on the American battlefield, it may be the right civilian disaster healthcare solution at precisely the right time.
A Happy Thanksgiving Wish for Everyone Out There on the Front Line
[Nov 20 07]
I recently read Hal Newman’s article
“Reflections on Life, Death and EMS.”
I am a Healthcare Disaster Preparedness guy and as such, I am a layman in
the area of First Response. When I thought about Hal’s EMS colleague who
took her life, I wondered if it would have mattered if she had recently read
a letter of thanks from a grateful citizen. I also wondered if she knew the
extent of the good she did while she was with us and how many lives she
touched and enhanced during her life.
You make a real difference in this world. Granted, it may be one patient,
one fire, one burglary or one accident at a time, but we would all be in big
trouble without you. You resuscitate us, rescue us, protect and defend us
when we need you the most. I have always believed that in order to be truly
happy, we must make positive contributions to mankind. Hal’s colleague
undoubtedly made significant contributions to the human condition and saved
many lives during her service. In one regard, I understand some of her
depression and sense of hopelessness.
When I served as the only medical supply officer in the Republic of Turkey,
I felt isolated, totally alone and most of all I felt an acute sense of
responsibility for things I really could not control. I worried constantly
about the possibility of losing a patient due to my lack of resourcefulness
in getting emergency supplies into Turkey before it was too late. The
feeling of having an overbearing weight on one’s shoulders is horrible and
it can be too much to bear. I have no any idea why or how I made it through
my depression. I do know that many friends saw my isolation and my sadness,
and tried to help me. A also know that my self-imposed exile frustrated many
of the friends that offered their support.
I discovered that in my good times I was very generous to others, but in my
bad times I withdrew from all those I loved most in order to suffer alone.
If my story sounds familiar, please try to get help to break out. For some
reason still unknown to me, God wanted me to continue my life’s journey. I
do my best every day for the people I serve, and for those I’m lucky enough
to mentor, hoping that in some measure, I can repay the gift that is my
life.
My wish for each of you on the front lines of health, safety and security is
that you can give yourselves credit for all the good you do and for the
lives you touch and save every day. All too often we hold ourselves
responsible for our shortcomings and forget about all the people who are
still with us and still need us. Perhaps the most important service you
provide to all of us is your mentorship. You will teach, mentor and affect
countless others in your career fields and pass on your passion to future
generations- be here for them.
Please, when you feel overwhelmed, use the support services available to
you. Also, please know that others in your field will be just as ready to
give you a hand as you would be to extend your hand to them. Take them up on
their offer. Continue to live, love, teach and serve. Pass your passion on
to the next generation of selfless contributors. You make such a huge
difference to all of us.
Happy Thanksgiving! Be well… and take care of yourselves.
Sincerely,
Jim Rush
I want to share an article I wrote for the
Association for Healthcare Resource and Materials Management (AHRMM) with
the readers of Big Medicine. There is absolutely no question in my mind that
emergency managers possesses experience and training that is priceless to
both Healthcare and Public Health leaders at all levels of government. The
ongoing emergency response to California’s wildfires is a vivid example of
the type of integrated response that jurisdictions across America should
emulate. While the economic and personal losses are horrible, we can only
imagine the losses in human lives if California’s emergency management
system was less well refined.
I believe that emergency managers can leverage California’s superb
performance and lessons learned to lead the effort in integrating Healthcare
and Public Health entities with the Emergency Management Agency in preparing
for and responding to a future Influenza Pandemic.
- JR
The Materials Manager's Role in
Pandemic Preparedness
[Oct 26 07]
Recently in healthcare, there has been an increased awareness that should a
worldwide influenza pandemic break out, American healthcare services would
be overwhelmed in the early stages of the public emergency.
A show, recently broadcast on The Science Channel, depicted how a pandemic
might begin in Southeast Asia and then spread rapidly across all parts of
the world infecting hundreds of millions of humans worldwide and leaving
tens of millions dead in its wake. It was striking to see how empty the
streets would be and how the normal hustle and bustle associated with
everyday life would disappear. It was also alarming to think about the
amount of trash that would be left behind as up to 60% of sanitary workers
would be either at home with the flu or afraid to report to work because of
the risk of becoming exposed to a deadly strain of influenza.
MEDLOG Inc. has been advocating a systems approach for pandemic preparation
for a number of years. Using this paradigm, the public health department
would provide the majority of the “hands-on” care as part of the “Pandemic
Community Surge.” This would ensure valuable hospital resources would be
conserved for “the sickest of the sick” (those strong enough to pull through
with intensive care equipment). Whether or not this paradigm is adopted by
the Department of Health and Human Services (HHS), there is little doubt
that materials management professionals will need to take leadership
positions in healthcare readiness.
Materials managers know that building huge stockpiles of medical supplies
and equipment is unrealistic for a few reasons:
1. “Just-in-time” supply systems function very well only as long as
healthcare purchasing patterns reflect actual usage. When large inventories
are built, the reorder point may reflect stockpile replenishment instead of
actual usage.
2. Financial constraints make investments in inventory untenable.
3. Few healthcare organizations have the space to store massive quantities
of food, medical supplies, pharmaceuticals, and ICU equipment even if
federal money was available in the hundreds of millions of dollars that
would be needed to fund the massive effort.
So what role can the healthcare supply chain professionals play in preparing
their organization for a Pandemic? The answer is significant.
What many materials managers may not know is that the HHS already offers
modest financial help in the form of Hospital Preparedness Program (HPP)
grants. HPP funds are intended to assist healthcare organizations better
prepare for “medical surges” in patients associated with man-made and
naturally occurring disasters like hurricanes, tornados, and yes, even a
pandemic. In the past few years, the Centers for Disease Control and
Prevention (CDC) has been funding state, territorial, and even a few major
cities’ efforts to become better prepared for a pandemic through one of
their major grant programs. Is some of that money available to hospitals as
they prepare for surges in the patients and fatalities associated with a
pandemic or even an outbreak of SARS? The answer is maybe.
So what can you do to best prepare your organization for operating during
and after a disaster? Whether your title is Supply Chain Manager, Director
of Purchasing /Procurement, Materials Manager, VP of Medical Logistics
Management or any other title, the healthcare organization will look to you
for supplies, equipment, and services throughout a pandemic. Here are a few
actions you can take to better your organization's preparedness:
1. Establish a close relationship with your organization's disaster
preparedness coordinator/emergency management coordinator. It is imperative
that materials mangers be brought into the planning process sooner rather
than later.
2. Evaluate the assumptions relating to the availability of goods and
services that have been built into your organization’s emergency management
plan (EMP). Consider whether these assumptions are likely to be valid during
peak demands for materials and services during a pandemic. For example, if
your organization’s EMP assumes that federal supplies and equipment will be
available to sustain hospital operating functions during all phases of a
pandemic, your EMP is currently incorrect.
3. Understand the phases/waves associated with a pandemic and evaluate the
demand for medical and non-medical supplies, equipment, pharmaceuticals,
food, and all contractual services during each pandemic phase.
4. Provide supply, equipment, and services subject matter expertise at
emergency management planning committees, exercises, and other hospital and
community pandemic preparedness meetings and events.
5. Accompany the Disaster Coordinator to local disaster coordination
meetings sponsored by the State Public Health Department's Bioterrorism
Coordinator (BT Coordinator), especially pre-proposal federal grant
meetings. You can then assist in writing the Hospital Preparedness Program (HPP)
grant proposal for submission to the state public health department. Once
HPP funds are approved, it is important for the materials management teams
to order and obligate HPP funds in the most expeditious manner possible.
State health departments as well as federal grant program project officers
track the obligation of grant dollars. Rapid obligation of grant dollars may
not assure better funding considerations in future years, but tardiness in
obligating funds may hurt.
6. Use AHRMM‘s disaster readiness information as a basis to help plan for
events depicted in the
community HVA
and use AHRMM’s Disaster Preparedness Manual for Healthcare Materials
Management Professionals to receive greater detail and “how-to” assistance
on the 10 functional areas listed in this article.
7. Be the leader in your organization for developing requirements lists for
disaster-related goods and services (a sample requirements worksheet is also
included in AHRMM’s Disaster Preparedness Manual for Healthcare Materials
Management Professionals). The earlier requirements are developed the
better. Consider healthcare infrastructure requirements such as back-up
generator fuel, water re-supply services, and regulated medical waste
challenges associated with a pandemic. During an emergency the
jurisdiction’s Public Health Officer in coordination with the Governor’s
office may order quarantine. Special convoy arrangements may help ensure
vital resources get through to the hospital.
Regulated Medical Waste (RMW) stored in and around the healthcare
organization for long periods of time can pose a significant health risk for
staff, patients, and the community. Onsite treatment systems backed up with
emergency power may be the best option for normal RMW treatment operations
and during a pandemic. While federal grant programs will not provide onsite
RMW units for normal RMW operations, “add on” units or autoclaves may be
funded through the pandemic or HPP grant programs. These will facilitate the
treatment of RMW surges associated with a pandemic or other disasters that
generate large quantities of RMW.
8. Fortify your organization’s supply chain management program. Work closely
with prime vendors and suppliers to plan for surges in demand for medical
products. Consider national distribution centers and how suppliers can
harmonize their supply chain with the phases/waves of a pandemic as it
crosses America. Here, your competence, experience, and resourcefulness as a
materials manager will shine through.
9. Become an advocate for healthcare preparedness at local, state, and
regional materials management planning work groups and at AHRMM state
chapter meetings. Share the strategies you learn with your colleagues and
other materials management professionals.
10. Develop memoranda of agreements with DOD active duty and reserve
organizations within the state/territory for logistics support during
disasters. Local DOD elements may be able to offer helicopter or fixed wing
transportation services for supplies and equipment from distributors to
hospitals when roads are impassable. The same agreements should be explored
with air taxis within the jurisdiction or region and where feasible with law
enforcement agencies for supply convoy escorts.
Every materials management professional has the opportunity to make a
phenomenal impact on how their organization will effectively function during
a possible future pandemic and other disasters and public health
emergencies. Those who take an active leadership role in developing
requirements and establishing new or broader contractual arrangements with
suppliers and community resources will be providing an invaluable service to
their patients, and their communities. Today’s healthcare organizations are
making decisions now on whether or not to organize for an emergency well in
advance. In the event of a disaster, the buck will more than likely stop
with the materials manager, so we better be ready.
Pandemic Planning Shortfalls - Culture of Scarcity
[Oct 8 07]
I thought I'd add my two cents on shortfalls
in America's preparedness to deal with the Pandemic that experts agree is
coming sooner or later. I will continue to advocate building Federal Reserve
Inventories (FRI) to bolster our food, chronic illness medicines, and
medical supplies and equipment supply chains during National catastrophes
like a Pandemic or a nuclear attack on a large American population center.
FRI will keep the supplies coming during future crises and will keep America
from developing a "Culture of Scarcity" which could be devastating to our
people and our economy. I though I'd share some experience that leads me to
worry about our societal expectations regarding necessities of life in a
National crisis. Since product rationing during World War II, we have never
had to endure severe and long lasting outages of products or services that
we have come to expect in modern day America. That in itself can be a huge
National challenge.
In 1977, I volunteered for an Air Force position as the Chief, Medical
Logistics Management for our healthcare facilities and medical aid stations
in the Republic of Turkey. Because of the tensions between America and
Turkey over the Turkish invasion of Cyprus in 1974, the US imposed sanctions
on Turkey, and in turn, Turkey closed all commercial shipments of goods into
the Republic needed to support our Service Members, their families and Armed
Forces healthcare facilities, commissaries and Base Exchange shopping
centers.
The closure of commercial transportation channels necessitated that the
shipment of all goods including food, consumer items, medical supplies,
vaccines and equipment entering Turkey come through military airlift and sea
lift channels only. It was a time of hardship for Servicemen and their
families. By the time "Yours Truly" arrived, there had existed for some time
what I call a "Culture of Scarcity" in the Armed Forces communities
throughout Turkey. I experienced logistics management challenges every day,
and observed some intriguing insights into how we Americans handle scarcity
of food, medical materials and essentially every consumer product group
during tough times. That 1977-1979 experience gave me a unique glimpse into
what America could become during a Pandemic or other National catastrophe.
You name it, we were out of it. I saw a woman in the Air Base supermarket
(the commissary) with a full shopping basket of canned yams. I happen to be
both inquisitive and a logistician, and I just had to ask her why she had
cleared the shelves of canned yams. She was both open and unabashed in
telling me that she and her family hadn't seen a can of yams in their first
6 months in Turkey. So, she was building an 18-month inventory safety level
that would provide uninterrupted yams to their table until they rotated back
to America.
When regular house fans came into the Base Exchange (BX), the Air Base
equivalent of Walmart, there would be a line around the corner a few hours
before the BX opened. I asked a medical material team member how folks knew
that the fans were arriving that day. He told me there was an informal
communication system with high placed BX insiders. I asked "You mean to tell
me there's an inside source for 15 inch oscillating fans?"...you bet, he
said. Large water containers like the type they use to pour water over the
winning coach's head at the end of a football game were also very hard to
come by. The same thing was true of space heaters, toys of any kind, all
food and above all else, bicycles...they were really hot items. Any kind of
bicycle.
Electricity was always a "maybe" - something you couldn't take for granted.
The first week there, I lost all of the contents in my side by side
freezer-refrigerator due to an 18 hour power outage. Pretty soon I learned
that compressors really don't do well with variations in electric current,
called brown outs, so the refrigerator-freezer didn't last very long. I know
from experience that candles aren't romantic after the first ten power
outages...they are just facts of life.
I could have written a book on how to shave in the dark without water. I got
pretty good at it and did it several times per week for some time. It seemed
that electricity outages also meant no water pressure since pumps use
electricity...made sense though. Drinking water had to be personally
chlorinated, and we handed out baby medicine droppers to Servicemen and
their families which were used to drop a set number of drops of Clorox per
gallon of water. You needed two water containers, one for the water where
the Clorox was still doing it's job of chlorinating and the other container
for the water that had met the required time for full chlorination. The kids
were great at pointing out the good water from the bad water containers.
The real horror for me came when I realized that we had a minimum of 13
folks (most of them children) on rabies vaccine at any one time. Getting
vaccine released from "customs impoundment" was a real challenge and
ultimately my obsession. Everything was impounded until the Turkish customs
officials cleared the shipment....and nobody knew when the inspector would
arrive, if at all, the day of the shipment. I worried
all the time, because I knew that while I was just an ordinary Air Force
medical logistician, I was all they had in Turkey and I was where the buck
stopped on medical supplies and equipment. Failure to find ways to get the
supplies into Country and released from customs to my customers throughout
the Republic could very well result in the death of those who depended on my
team. Part of my daily regime like brushing my teeth and shaving was saying
a prayer asking that none die due to the lack of medical supplies or
equipment.
We lost several shipments of Polio vaccine and Diphtheria, Pertussis and
Tetanus (DPT) vaccines due to the impoundment of the vaccines and their
spoilage in the impoundment yard. We were living very close to the edge,
keeping up with the demand for lifesaving medical products, but we were in a
disciplined society. In today's America, what effect would these long term
and persistent shortages have on the fabric of our
society?
If we have knock down drag out fights over "Tickle Me Elmo" dolls at
Christmastime, and long lines for I-Phones, imagine life during a Pandemic
when anxious parents are waiting for infant formula outside supermarkets and
drug stores when the supply trucks arrive with far too few supplies. You
might ask "Why would we be out of common items during a Pandemic?" There are
two main reasons.
1. Breakdown of "Just-In-Time" Supply Chain Management. Our food, gasoline,
pharmaceutical, consumer products and medical supply chains work pretty much
the same way as our monetary systems....on faith that the materials will
always be there for us. The folks have faith and trust in our financial
systems, and so we don't see everyone across America withdrawing their money
from banks when the stock market or currency markets fall in value. The same
thing is true with our other commodity groups. Typically, we only purchase
what we need for a few days to a week or so. For pharmaceuticals, we
normally have a portion of a month's supply of the drugs that maintain our
heath. We are not living in a "Culture of Scarcity," so the supply chains
work beautifully based on very long, very accurate product consumption
histories.
The Onslaught- When the first report comes out from the CDC that a "Novel
Strain" of Influenza has arrived in North America all of us will take
inventory of food and water, cold and flu medications, chronic illness
supplies and pharmaceuticals and most of the other items we have around the
house. We all know what happens when a large segment of the population
decides to stock up on the same items at the very same time. We see it in
some cities when the weather service predicts a 3 inch snow event....bare
shelves.
Imagine the rush to re-supply medicine cabinets all across America during
the same week. As store shelves empty out, we become a bit less confident in
our supply system, so, by golly, when we see items we need..... or think we
might need, we buy them...lots of them. That siege mentality of purchasing
drains the supply system dry, since no demand forecasting program can
predict a Public Health emergency or the Public's reaction to it. The buying
trends are based on fear and not prior week's consumption. As the purchases
vacillate wildly, so do the re-supply orders and the supply chain is unable
to function as advertised. It is then that we become a "Culture of
Scarcity". Instead of having to stick it out for a few days in a snowstorm,
we are looking at a long term situation...long after the Pandemic fades -
perhaps 3-5 years for accurate consumption trends to emerge and supply chain
recovery. Until then, the Just-In-Time supply system will fail over and over
again, trying to make sense of erratic demand for products.
2. Culture of Scarcity. It is impossible to predict right now, how
American's will behave when there are shortages of everything we take for
granted in today's America. We can only hope that we don't become a society
of looters and roving gangs of opportunistic thieves. The only thing that I
believe that can and will short circuit the Culture of Scarcity is a
confidence in our Government's ability to flow life's necessities through
established supply chains during National catastrophes. If the Federal
Government signals an inability to sure-up the food supply, fuel supply, as
well as the Healthcare and Public Health Infrastructure, "Katie bar the
door!"
During a Pandemic or other large scale catastrophe, Federal, State and local
elected officials can urge calm all they wish. But when the kids are hungry
and Uncle John has run out of his pharmaceuticals that manage his mental
disease, times will get very bad... and very fast. The answer isn't for each
American to build large caches of everything they use in their daily life -
in fact that would cause more harm than good. If every American had a three
month supply of every product from toilet paper to pharmaceuticals, to meat
and canned vegetables, distributors would start to see unforecasted and
sporadic large spikes and severe drops in demand for products. What would be
going on, would be 300 million Americans replenishing their supply caches -
all using different reorder points. What happens in this case is rolling and
persistent backorders of everything, because there are no societal shopping
trends like the ones most of us use today. These trends are the basis for
demand forecasting and are the pillars of a Just-In-Time supply chain.
Without solid predictable ordering patterns, our "Just In Time" marketplace
begins to disintegrate.
The only real solution is for Government agencies to invest in and oversee
the management of sufficient supplies of "life-necessity items" and
pre-position the Federal Reserves at the "Wholesale Level" - in other words,
at civilian distribution centers. During normal conditions, America's
distributors could stock rotate very large quantities of Government-owned
products in a way that would result in near-zero losses of the taxpayers'
investment in inventory due to expiration in storage. In a crisis, American
confidence in it's supply structures would remain high, thus reducing the
threat of descending into a Culture of Scarcity.
By maintaining adequate Federal reserves of life's necessities....and
releasing some reserves during even the regional disasters like hurricanes
and earthquakes, we can demonstrate the dependability our supply structures,
further bolstering American's confidence. Is this a tall order? You betcha!
Can this be accomplished? You betcha.
Such programs can work very well if they are managed correctly. The
Government has been maintaining a Strategic Petroleum Reserve for many years
and the oil has been replaced as it was rotated out to refineries.
In a crisis, American life doesn't grind to a halt as soon as we all fill up
our gas tanks and oil storage tanks. We can and really must initiate the
same types of reserves for food, pharmaceuticals, medical supplies and
equipment and other critical life support products.
Can we start now?
Establishing, Provisioning and Managing Special Needs Shelters
Have you been loosing sleep since reading report after report on the inadequacies of shelters to care for persons with special needs during the 2005 Hurricane season? If so, you are not alone. You may take comfort in knowing that you are among the distinguished company of many good and decent Emergency Managers across America. During hurricane Katrina, I found myself asking “How can we call ourselves a great and compassionate Nation when we fail to care for the most vulnerable among us in the worst of times?” The answer I arrived at was “we can’t.”
For the general population, we pretty much have the needed food, water, clothing and shelter items down pat. However, what about the growing ranks of citizens with special needs, now estimated at one fifth of America’s population? The challenges must be significant since we often can’t even agree on the definition of special needs populations.
Why don’t we forget about defining specific groups of special needs folks and let them self-identify? Instead, perhaps we should define specialty sheltering items and services available, and leave it at that. We might want to just say, “Specific shelter locations for persons with special needs will be designated and advertised in regular communications with the general public and persons with disabilities advocacy groups. Special Needs shelters will be provisioned with the following: medical and non-medical supplies and equipment, pharmaceuticals, nutritional products, and personal assistants and interpreters (which may be required during sheltering events by non-English speaking persons or persons with chronic diseases or physical, emotional or psychiatric disabilities).”
While that statement is easy to reduce to writing, the processes needed to determine which items should be stocked, how many of each item to stock and how to conserve the community’s investment in inventory (by avoiding product expiration in storage), are not as easy. Recruiting sign language specialists, interpreters and medical assistants are also challenging tasks. Below are some suggestions which may be of value when planning special needs shelters:
- Select and plan for a shelter for Special Needs populations based on the experience of others. The best advice one can heed is to communicate with shelter managers and support staff that have first-hand, “on-the-ground” experience from the 2005 hurricane season. There are hundreds of persons who know the types of facilities and materials and services needs that were not met as well as the work-arounds that had to be employed. The lessons they learned the hard way can help planners avoid repeating past mistakes.
- After designating the special needs shelter, get the word out.
Public service announcements are a great way to get information out during community or statewide exercises. In the PSA, consider specifying the types of services that will be provided in each special needs shelter and the personal items evacuees need to bring with them. Another way to reach persons with special needs during a disaster is through advocacy groups. Consider flyers, press releases and newsletters as good ways to publicize which shelters are designated to care for persons with special needs and the particular goods and services offered at each shelter location. Advocacy groups should be brought into exercise planning as well as designating shelter locations for persons with special needs. During exercises, your advocacy group partners can be invaluable in getting folks with special needs to the shelters providing the goods and services people require.
- Determine who will be the likely populations to show up at the shelter and anticipate what their needs will be.
It may not be necessary to develop “qualifying criteria” for the shelter. In the end, if a person self-identifies that he or she has special needs during disaster sheltering operations, the shelter manager will have to take those special needs seriously with or without a special qualification. Some states are developing “registries” where persons with special needs can sign up in advance. Due to privacy concerns, each State and Territory public health department should have involved specialists in patient confidentiality and the requirements of various Federal regulations regarding privacy. The Health Insurance Portability and Accountability Act (HIPAA) of 1996 has specific requirements regarding the privacy of a persons health records which may pertain to special needs shelters.
Special Needs persons, including folks with disabilities and the elderly, will need a host of support services. For example, in an evacuation, a person who was receiving wound care from home health professionals will need to know which shelter locations will be staffed and supplied to provide wound care. A person who uses diabetes supplies and insulin may not have sufficient supplies to endure a lengthy stay in an evacuation shelter.
Persons who rely on psychiatric medications did not receive adequate support during hurricanes Katrina and Rita according to the National Council on Disability (NCD). Their findings: “THE NEEDS OF PEOPLE WITH PSYCHIATRIC DISABILITIES DURING AND AFTER HURRICANES KATRINA AND RITA”: POSITION PAPER AND RECOMMENDATIONS; National Council on Disability, July 7th, 2006. Now I have read scathing indictments on Inspector General (IG) and the General Accountability Office (GAO) reports in the past, but nothing ever came close to the ones listed at: http://www.ncd.gov/newsroom/publications/2006/peopleneeds.htm To make matters worse, the NCD is a federal policy agency, and there is little to suggest that significant progress has been made across America since 2005 in sustaining persons with psychiatric disabilities.
4. Determine the specific supplies and equipment required by the special needs shelter.
We know there are literally hundreds of reports, papers, studies and all manner of well intentioned works in the Public Domain regarding the subject of caring for folks with special needs. I have been unable to find a single report or study that lists the processes that may help Emergency Managers decide what items to include, how to arrive a quantities of medical and non-medical supplies and equipment to manage and how to get the products and services to the right place at the right time. I thought I’d step out into the discussion and list some concrete steps that my be taken by Emergency Managers who want to make the 2005 Hurricane season a horrible but non-recurring nightmare.
ü Recruit a subject matter expert (SME) team consisting of healthcare specialists in Disabilities, Emergency Medicine, Geriatric care, Psychiatric care and long term patient care. Although nurse specialists will select most of the patient care items, it may be a good idea to recruit a physician as the SME team leader. Prepare for success by selecting a strong leader for your formulary and special needs development team. A pharmacist will be the SME member who will extremely helpful in the standardization and cross referencing of medications. The reality of life in a shelter operation will dictate a “lean formulary” and the pharmacist will be invaluable in areas of drug interactions as well as using standardized substitute drugs. A respiratory therapist and a dietician (for special feeding items) would also be good choices as team members.
Last but not least, recruit a healthcare purchasing agent or a materials manager as the person who will provide sources for the various products on your formulary listings. The SME team will need to concentrate on standardizing items in order to meet needs but keep the requirements lists manageable. The purchasing agent or healthcare materials manager can play a supporting role but you need a strong medical person as the formulary development leader, since many formulary choices will be difficult but essential.
ü Divide your formularies and services into categories, since this will make vendor selection and advocacy professional group reviewers tasks easier. Food and special feeding items, medical surgical supplies, medical equipment, pharmaceuticals, patient care and apparel and hygiene needs are some of the commodity categories SME teams will need to consider. Just some categories of needs and products include:
A. Materials
- Respiratory care
- Wound care
- Specialty care-Ostomy products
- Pharmaceuticals-chronic care medications
- Patient shelter hygiene supplies
- Mobility items; wheelchairs (regular and wide), walkers, crutches, etc.
- Special nutritional products, infant formula (including non-dairy), enteral feeding products (for persons who can’t swallow and have a feeding tube).
- Specialty cleaning and care kits (tracheotomy, ostomy,)
- Bariatric care (obese persons), bariatric beds, wheelchairs, special lifting devices (Hoyer lifts and associated equipment)
B. Services
· Redundant notification systems to notify persons with disabilities that an emergency exists and all pertinent actions that need to be taken
· Special assistants for the blind.
· Special assistants for the deaf and hard of hearing including couriers for notification.
· General services shelter volunteers
ü Select distributors for materials. Most state and territorial Public Health agencies have separate vendors (often called prime vendors) for major product categories such as; vaccines, pharmaceuticals, medical supplies and medical equipment. When allowable, it’s a good idea to piggy back onto existing state contracts for special needs shelters instead of letting new contracts. This is because the shelter manager can leverage the jurisdictional purchasing power and often obtain existing jurisdictional contract pricing and terms. Since the Public Health agency is normally the provider of supplies and equipment for special needs shelters, the additional materials can be added to the existing contract by using a contract amendment. The public health purchasing agent can work with the state contracting officer on any contractual issues involving special needs shelter acquisitions, delivery and billing information. The key in this area like all other emergency management functions is advance work. Those Public Health agencies that wait to develop formularies and arrange contractual details until an actual disaster is underway will most likely be the ones calling FEMA immediately for help. Also, in large scale disasters, there may be system-wide supply and equipment shortages.
ü Recruit and train special services staff. Advocacy groups for persons with disabilities and other special needs people may be able to help the special needs shelter manager identify companies which provide services to persons with disabilities. Non-governmental organizations including the Red Cross, Salvation Army and Goodwill Inc. as well as faith-based congregations may be able to provide volunteers. Whether the persons who will staff the special needs shelters are paid or unpaid workers, the identification and training components must be accomplished beforehand in order to succeed.
3. Conclusion. The special needs of persons with disabilities and other vulnerable persons will exist whether or not State and Territorial Emergency Managers and Public Health Officers plan for the needs in advance. Advance planning will make a difficult situation manageable. The lack of advance planning will not only be a disgrace and will likely cause pain, suffering and perhaps deaths.
Throughout my career in healthcare, medical logistics and emergency management, I asked myself if my planning would be sufficient for my mother and sisters should they require sheltering in a disaster situation. In the end, persons with special needs are indeed our community family. Good enough doesn’t cut it for family and shouldn’t be “good enough” for our community members, especially the vulnerable. Planning for and submitting our requirements and the associated budgetary figures to the appropriate funding authority may not result in all requirements being funded. What it will do is demonstrate that you took the time to determine what is needed, you articulated the needs in writing to the funding authority and as funding was made available, you provided for the needs of our community, including our most vulnerable persons.
Training Citizens for Disasters
[Jul 31 07]
One of the many hats an Emergency
Manager must now wear is that of a trainer. Communities need
training and familiarity with procedures that work in every day life
as well as disasters. For years, we have had pretty much the same
scenario of actions following an incident: first response, triage,
on-scene stabilization and transportation of casualties to the
appropriate level of care. So a question may be: “What additional
steps can be taken by Emergency Managers to prepare the community
for the real thing?” One answer to that question is “Community
Familiarity Training”.
In any disaster, members of the affected community will ask, 'what
do I do?' and 'where do I need to go?' The Emergency Manager can
make a real impact in both exercises and actual emergencies by
putting all the elements of the Community “Emergency Management Plan
(EMP)” into effect. The bottom line is, the more familiar the
community is with the “Where to?” questions the less ad hoc and
“on-the-fly” arrangements need to occur and the smoother the
disaster exercise or a real event will go. In the real event,
communities which practiced the procedures outlined in the EMP will
benefit from the exercises and will have better outcomes. The
following is a brief description of some of the questions that can
be practiced during exercises.
1. Where do I go in a disaster to give blood? Why not coordinate a
blood drive with the American Red Cross for each and every disaster
exercise? As a part of each exercise planning meeting, consider
including the Red Cross folks to coordinate a number of blood donor
drives at well known centers throughout the community. In most
cases, the community knows where the every day blood collection
centers are located, but haven’t associated these collection centers
with actual disasters. It is amazing how many blood collection
opportunities are lost because local, state and regional disaster
exercises did not include a blood drive. It’s not only the community
which will benefit from exercise blood donor centers. The Red Cross
may want to exercise their blood processing and transportation plans
as a part of the community exercise. We all know that America’s
blood supply can be extremely lean at times, resulting in special
Red Cross media requests for donors of specific blood types.
Ultimately, local, regional, and regional exercises could result in
a cross leveling of the American blood supply. The local Red Cross
director or the Red Cross Biomedical Services unit may also be able
to assist Emergency Managers in the identification and ordering of
blood products and tissue from the nearest blood products and tissue
banks. These types of products will be in demand during London or
Madrid type bombing events or in treating survivors of a nuclear
detonation.
2. Where do I go to receive food, water and other emergency
supplies? Here is another opportunity to make routine operations the
Emergency Manager’s friend. If the Emergency Management Agency
intends to set up food and water dispensing locations in the parking
lots of large retail stores and or in supermarket parking lots, set
up mini-dispensing sites there during exercises to hand out
information flyers regarding personal and family preparedness kits
and a home emergency provisions cache of food, medical supplies and
other emergency essential items. The folks will begin to equate an
exercise with the dispensing areas and hopefully, it will become a
part of the community’s consciousness.
3. Where do I go to drop off donations of food, clothes, toys etc.
Donations are common headaches for Emergency Mangers since all
manner of products pour into disaster relief centers making the job
of sorting, accounting and distribution more difficult that it needs
to be. In this case consider modeling the gift commodities groups to
the recycling program. We are all trained to know what products
(glass, plastics and paper etc.) to place out during set recycling
days. If during exercises, individual commodity donation centers are
set up at well known locations, the public will begin to understand
where the food centers, clothing centers etc. are set up and will
begin associating locations with commodities.
4. Where are evacuation shelters? And which shelter is right for me?
Public Service Announcements (PSAs) are a great way to get
information out during community or statewide exercises. Local radio
and television stations are a great source for recruiting on-air
personalities and PSA production folks to help get the word out to
the community on a wide variety of emergency-related topics. “PSA
spots” can be aired in conjunction with FCC required emergency
system tests. In this way, the Emergency Manager’s information will
get attention since the Public’s attention is already focused on the
emergency test. In the PSA, consider specifying the types of
services that will be provided in evacuation shelters, where special
needs shelters are located and the personal items evacuees need to
bring with them.
“Special Needs” shelters will need to be established along with
supplies, equipment and services for persons with disabilities and
other segments of each community including the elderly. We all know
that information is plentiful regarding personal preparedness steps
all citizens should be taking regarding a supply of chronic
condition medications and supplies. Still actual experience during
the 2005 hurricane season illustrated the need for community special
needs sets and assemblages for use during disaster evacuations.
Right after this article, we will be submitting a special article to
“Big Medicine” with suggestions for developing formularies, Prime
vendors as well as service requirements and special equipment sets
along with suggestions on how to maintain the items in storage and
transport them to the Special Needs Shelters.
Educating the Public on what to do, where to go and what to bring
with them in disasters is a never-ending role of the Emergency
Manager. By looking for novel ways to deliver the message and inform
the Public during exercises, the Emergency Manager will be making
deposits into the Community memory bank. During actual events, that
bankroll of knowledge will pay huge dividends.
[Jun 30 07]
Sometimes I find myself fondly remembering the good old days when Community Emergency Management seemed to be a fairly straightforward function, but today things have definitely changed. There are now many more players with a role in emergency response which Emergency Managers must help integrate into their jurisdiction’s total disaster response effort.
If you have asked yourself “What can I do to assist Healthcare organizations and Public Health departments integrate into a jurisdiction wide All Hazards response team?” the answer is you can do a great deal.
I’m afraid what we have today is an old paradigm being applied to a new reality. First responders rescued casualties, provided emergency medical attention on the way to the hospital and handed off casualty care to the hospital. Hospitals had decent staffing levels and the medical materials to accept the additional casualties. The good old days are gone.
In 1974 when I first entered the field of Healthcare Disaster Preparedness nearly every hospital had a warehouse. Demand forecasting was an exciting future promise in Materials Management but was not to become a reality for another 10 years or so. Nearly every hospital and medical center had enough supplies to keep clinicians supplied for anywhere from 30 days to three months.
Healthcare staffing, including nurses, nurse assistants (I don’t remember certified nursing assistants back in those ancient times) and support personnel staffing levels, were much more generous in the good old days.
Today, healthcare staffing is extremely lean, and in many cases around America the medical profession is losing too many caring people who say that Healthcare has become much more about the bottom line than it is about care.
Today, managed care, reduced Medicare and Medicaid reimbursements accurate demand forecasting of medical products through computerization, and what has become known as “Healthcare Supply Chain Management” has changed Healthcare’s ability to manage a disaster-related surge in casualties dramatically. The financial pressures on Healthcare are immense and everything must be “optimized.”
In staffing, the questions starting back in the 80’s became, “what is the optimum nurse to patient ratio?” Can registered nurses become “care team leaders” and become more of a manager than a caregiver?
In Materials Management questions were asked “How can we optimize our inventories?” “How can we drive costs out of our purchasing plans?” How can we minimize our medical product inventories and the associated dollars tied up in inventory?
The bottom line question is “Aren’t these costs containment measures and a Just-in-Time” supply chain strategies a good thing?” The answer is:” As long as nothing unanticipated happens and if staffing levels reflect the true patient care acuity levels, it can be a good thing”. However, if something unanticipated happens…..lets say a disaster, healthcare can become almost instantly overwhelmed.
Will hospitals and medical centers close down and defend in place once patient capacity is reached?
What will Emergency Managers do with casualties when healthcare organizations reach full capacity and close their doors?
Perhaps better questions are, “What can Emergency Managers do in advance of the next disaster to help Healthcare and Public Health leaders in the community better plan for disasters?” and ”Is this mission impossible?
In the “Mission Impossible” series, the voice on the disintegrating tape recording said “your mission if you chose to accept it…” Well, here are a few suggestions that may be helpful to you, if you choose to take on the role as a true integrator and make yours a mission possible.
- Include Healthcare and Public Healthcare in all jurisdictional planning. While the Joint Commission (TJC) for Healthcare Organizations has included standards for disaster preparedness for years, the healthcare organizations got into a bad habit of just going through the motions in planning, training and exercising to meet or exceed the TJC standards in order to be accredited. You can help healthcare leaders develop a true “Readiness Mindset” in planning for real world disasters based on your community Hazard Vulnerability Assessment (HVA). The healthcare folks need to know what events are most likely to occur and how many and the likely mix of casualties that will likely be generated under each event scenario.
Emergency Managers understand resource management and conservation of critical assets in a disaster. You also know that you can’t expend all of the jurisdiction’s healthcare assets in disaster-care and not be able to treat the heart attack, stroke and trauma patients until after disaster recovery. You can help healthcare leaders by brainstorming ways to incorporate all community medical personnel including urgent care centers, private physician practices, all medical materials resources, all non-governmental organizations including faith based organizations into a “Community Healthcare Expansion and Sustainment System.” You understand that in a disaster, the hospital or medical center is the last bastion of defense in caring for the sick and wounded. You understand multiple levels of response in a disaster battle plan. Healthcare and Public Health leaders across America need your years of experience in building robust disaster response systems more now than ever before.
- Use Healthcare competition to your advantage. Day in and day out hospitals and medical centers compete with each other for patients, specialists and staffing resources. All Healthcare leaders understand the value of protecting the healthcare or medical center and its staff in a disaster. As the word gets out that medical center A, B, and C are attending regular Emergency Planning meetings with the Emergency Manager and elected officials, it won’t be long before medical center D requests a seat at your table. The fact is the better and more robust a healthcare system is, the better it will respond and the faster it can come back on line with full normal services after a disaster. That alone is a potent incentive for any healthcare organization to integrate with the Emergency Management Agency and all jurisdictional response agencies.
In addition, most Public Health agencies will appreciate being involved in the jurisdiction’s planning and your experience in managing disasters. As you present concepts of Emergency Management including how the Incident Command System works, the Public Health folks will want to do their part and will grow from the experience you offer. Then, Healthcare and Public Health entities may begin to work together while sitting at your table.
- Understand that Public Health does not see “hands on health care” as their role. But, if there was ever a time for not drawing functional lines in the sand, now would be that time. Public Health has just recently begun receiving adequate funding after 30 years of mission reductions and funding stagnation. There are probably few Public Health Officers out there who have personal experience providing “hands-on” care to a community in a Public Health crisis. Don’t be surprised if your Public Health Officer tells you that during a Pandemic, all healthcare services will be provided by healthcare organizations. We all know that American Healthcare is in crisis and in some cities it is shutting down. If we as a People can’t find a way to build an integrated healthcare/public health response to the next pandemic, healthcare as we know it may also be a fond memory.
Let’s face it, the 1918 Pandemic was a long time ago and since then, Public Health Departments have concentrated on early detection, post exposure prophylactic treatment, immunization and mitigation measures like anti-viral medications. As you read your State or Territory’s Influenza Pandemic Plan, use a highlighter pen to mark up all the areas that address hands-on healthcare. Then see how many highlighted sentences and paragraphs you have. It is likely that providing healthcare to influenza patients receives very little coverage. The question that needs to be asked is where patients will go for treatment when hospitals reach capacity, exhaust staff or run out of supplies.
If you can implement just the five tips mentioned here, you will have not only done your job well, but you will have changed the entire culture of Integrated Emergency Management in your jurisdiction. Once you have all the stakeholders in the same room, facing the same scenarios and the associated casualty numbers, you should be well on your way to leading a true integrated community response.
- Integrate Federal Grant Funding Streams. This may well be the hardest and most contentious issue Emergency Managers will face. Federal Agencies are working on Crosscutting grant guidance but the concept is not as widely accepted as it needs to be.
There is no use in having a robust First Responder capability if the end result is hundreds or thousands of casualties being dropped off in hospital parking lots because the hospital’s capabilities have been exhausted. There is no use in developing fully compatible, redundant and highly survivable communications systems if the messages communicated during a disaster are nothing more than a litany of failures in law enforcement, healthcare, public health and municipal services. A jurisdiction must develop balanced system wide response capabilities if it is to have a successful disaster management system. The heavy lifting comes in when the Emergency Manager attempts to build leveled capabilities into the jurisdiction-wide integrated response systems. Grant proposals must depict activities in such a way as to demonstrate the interdependence of all jurisdictional disaster-related activities as an interrelated system which requires cross functional funding. The jurisdictions that can share grant funding as a community and not as a number of discreet interest groups will be the jurisdiction that provides outstanding disaster services to its citizens. The acid test of leadership and community cooperation will be evident on disaster day, or D-Day.
- And the most important for last: Only the Emergency Manager can develop competent plans for saving the lives of our most vulnerable citizens. Persons with disabilities and elder folks need all of the Emergency Manager’s skills, abilities and initiative to survive a catastrophe. I can’t imagine a caring person watching the scenes on CNN and FOX News where folks were abandoned and died on the streets and in doorways without feeling guilty that this could happen in 2005 America. We put a man on the moon in 1969 and yet, in 2005 we had to sit helplessly and watch dead bodies floating down streets in New Orleans. We can do so much better than that and we must do better than that. The Emergency Manager can lead the National effort to make those scenes just a bad memory never to tolerate that disgrace again in America.
Develop all the requirements and the line item by line item costs that are needed to sustain persons with disabilities and special needs at home, during evacuations and in evacuation shelters or healthcare centers. Then move the requirements and cost data upward as called for in the National Response Plan. The Emergency Manager can link the requirements to NIMS resource typing and can express how the requirements will be necessary in order to attain Target Capabilities and Universal Tasks. If the Emergency Manager cannot do this, it is extremely unlikely that anyone else in the jurisdiction can.
Finally I’d like to share a thought I had many times when I was stationed in the Republic of Turkey. As the Regional Chief of Medical Logistics Management and being at the geographical and literal end of the Supply Pipeline, almost every day presented challenges that I never had to deal with before.
To get though those days that stripped me of my boyish good looks I would say to myself… “You may not be all that good, but you are all the folks have and you have to get this done.” I hope each Emergency Manager reflects on that quote as they plan for communication, evacuation, and sustainment of persons with disabilities and special needs at home, in shelters or in care facilities during disasters.The fact is you are that good, persons with disabilities and special needs depend on you and you have to get this done.
Pandemic Planning: Why Healthcare and Public Health Aren't Talking
[May 11 07]
There is a lack of communication in America regarding Pandemic Influenza planning and resourcing, and it must stop immediately. The Federal leadership is putting out a loud and clear message that, in a Pandemic, the States and Territories will be pretty much be going it alone. That sounds great since the CDC grant programs are pouring money into State Public Health Departments so they can do whatever they need to do to pretty much “Stand Alone” during a Pandemic. So what’s wrong with the plan? Plenty!
The major problem that nobody wants to talk about is that America is unwilling or unable to address where sick Americans will get care during a Pandemic that Federal Agencies are saying will occur.
The Public Health Community is taking a three-pronged approach to managing a Pandemic.
- Early Detection. The idea here is to provide Public Health Officials with an early warning that a new “person to person” strain of Influenza has mutated from the current H5N1 strain. It is thought that the earlier we recognize that the Pandemic has begun, the better we can deal with it. Sounds good doesn’t it? Imagine the North American Aerospace Defense Command (NORAD) detecting inbound missiles coming in from an attacking country. Then imagine the President asking for options from the Commander in Chief NORAD, only to be told we didn’t have options until the new missile defense system came on line. Imagine the horror the President would feel if the NORAD folks said they had destroyed all offensive missiles because the new defense system would render all offensive weapons useless. Well folks, that’s about where we are now in Public Health. We spent a lot of money on syndromic surveillance systems so that we know a novel Influenza virus when we see one. The problem is there is very little we will be able to do about it when it arrives in the USA.
- Antiviral medications. The Centers for Disease Control and Prevention (CDC) has said “Four antiviral medications (amantadine, rimantadine, zanamavir and oseltamivir*) have been approved by the U.S. Food and Drug Administration (FDA) for treatment of influenza. However, you will need to begin taking the medication within 2 days after becoming sick.” What they don’t say is: (a) Does the CDC have enough antivirals on hand in the Strategic National Stockpile to cover the American people? (b) How is antiviral medication going to be distributed…and when? (c) What is the priority, either by medical condition or occupational category that local Public Health departments are going to use in administering the medications?
- Vaccines. If there is a magic cure for the new strain of influenza, it will come by way of a vaccine. The problem with the whole idea of vaccination is that it cannot be manufactured until the specific strain of the organism is present in the population. We hear that it may take 6-9 months for vaccine manufacturers to ramp up production of vaccines and start moving an effective vaccine through the supply chain.
The Issue: It is estimated by Federal Officials that about 45 Million Americans will need some form of professional medical care.
Problems:
Home Care. None of the above strategies discuss where the sick Americans can go to get the definitive care that Federal officials are saying they will need. Even worse, the other 45 million, give or take a few million, Americans are going to need to care for themselves or have family take care of them at home. Did anyone tell the makers of Robbitusin, NyQuil, VapoRub, Aspirin, Tylenol and the other manufacturers of over the counter (OTC) medications and other cold and flu home care supplies and equipment to expect a bit of a spike in demand for…let’s say a year or so? Do the drug store chains know anything about this? Do we think that when the drug store chains and supermarkets run out of OTC medications the folks who may have been able to stay home will now have to go to the ER? Pretty good bet isn’t it.
Hospital Care. Every time we open a newspaper or a magazine, we read that the American Healthcare System is in a state of crisis. With financial pressures from managed costs (oops! that’s managed care isn’t it), reduced Medicare and Medicaid funds, and an increased Baby Boomer population, our hospitals and medical centers have been at near capacity for some time now. Emergency room visits are up in many, if not most, areas of America. But as the saying goes; “You ain’t seen nothing yet.” In a Pandemic, when the shelves of OTC and home care products are empty, every ER in the country will be inundated. Or will they too run out of supplies?
Under the best of healthcare surge plans, we might be able to take on one million very sick patients that can be saved if they get immediate and aggressive intensive health care. Why only one million additional patients if hospitals cancel all elective procedures and go to 12 hours on/12 hours off staffing schedules?
I have seen figures that up to 40% of the nurses in the country will either be sick themselves or will be home taking care of loved ones who are sick. If America’s divorce rate is approaching 50%, would the 40% call-out seem reasonable?
The one million additional patients is just my guess; but someone has to guess.
While we are on the subject of hospitals, with all the elective procedures and outpatient visits cancelled for about nine months, how are healthcare organizations going to be reimbursed so that they won’t go out of business during that period? We absolutely have to answer the really tough questions. Now would be an excellent time to get the details out to the healthcare industry.
Medical Facilities, Supplies and Equipment. Has anyone in the Federal government met with manufacturers and distributors of medical supplies, pharmaceuticals and equipment? I like round figures, so let’s for the sake of argument say that 100 million folks will become infected with the new strain of influenza.
How long will manufacturers take to ramp up production of all OTC medications, home health supplies and hospital supplies? Can manufacturers expect to acquire raw materials on the global marketplace? Are the manufacturers planning to go to 12-hour shifts? Is there any excess capacity to surge manufacturing at all in six to nine months? I asked that question to the X-ray film manufacturers as a part of wartime surge planning. The answer was “maybe in 12 months.” It would take that much lead time to institute such changes.
Are those who are planning to open Alternative Care Centers (ACC) planning on developing a medical logistics support plan to support the ACC? Do healthcare Materials Managers know anything at all about this ACC Concept of Operations? What about food, water (drinking, washing, and chillers), back-up generators (and fuel), regulated medical waste (RMW) treatment units? Do RMW transporters and off-site treatment facilities know anything about a surge in RMW. If quarantine is ordered, how will transporters get into the quarantined jurisdiction to pick up and transport the medical waste? The hospitals that treat RMW on-site will be very happy about their decision process. Are pre-established, anticipated demand contracts in place for all hospital services?
What about opening previously shuttered hospitals? One would think that every Public Health Officer in the county would be submitting plans and budget requests for re-opening currently closed hospitals, or more likely, former hospitals that are currently being used as office buildings, county or state buildings. Well, you would be wrong. We need to put plans and teams together across America to upgrade previously operational hospitals to be able to support at least an intermediate level of healthcare during a Pandemic.
What about mobile medical facilities? In the 1960s, America had about 1900 “Packaged Disaster Hospitals”, each with three operating rooms and each with 200 beds which were capable of attaching IV poles and medical equipment devices. These were not cots; these were beds where nurses and physicians would not have to be on hands and knees to provide patient care. That was 380,000 additional beds and 5,700 operating rooms. Each one of these “Packaged Disaster Hospitals” came with enough equipment, pharmaceuticals and medical supplies to operate for 30 days without re-supply.
Healthcare Staffing. With about a 40% reduction in healthcare providers, how will hospitals cope with “The Longest Year” in American healthcare? Are Public Health departments conducting training for healthcare augmentees? What about the Red Cross? Are their contracts for “per diem” nurses amended to accommodate the surge in demand for care givers? Are communities and hospitals involved with their state or local Medical Reserve Corps (MRC) chapter? Is the MRC expanded to include home health providers? Are provisions to care for persons with disabilities in place at Public Health departments, healthcare organizations, and the state or local MRC? Are folks going to deliver back-up power units, food, water and assistants for Special Needs and At-Risk persons on life support equipment in their homes? Are all Non-Government Organizations being fully integrated into the Public Health Department plan for community surge?
Let’s not forget that in 1918 America had a very large contingent of faith-based care givers. How capable are America’s faith-based organizations to provide various levels of patient care and end-of-life care today?
And now for the $64,000 dollar question: Will Public Health Departments across America open emergency healthcare centers and provide “hands-on” patient care? The answer is…They had better! If the Public Health Officers across America are not planning to augment the healthcare industry, which everyone knows is at or near capacity (and in many jurisdictions is over capacity), that the next “After-Event” Congressional Commission will be asking the question “Why Not?” Is it a “It’s not my job” type of thing?
What I believe wholeheartedly is that the time for plans, studies, research projects and countless articles on Pandemic is over. This anticipated Pandemic is undoubtedly the most studied Public Health emergency in world history. Never before has a disease been so studied and researched, while the society in which it was studied remains so utterly unprepared.
I have developed a “Battle Plan” type of chart and enclosed it in this paper. This is just one person’s best effort at trying to hold the line during a Pandemic. Every Public Health Officer in America will have his/her own plan. At least I hope they will, for the sake of the citizens within their states and territories.
JIM RUSH

James M. Rush, CHPM, is the Vice President and Chief Operating Officer of JVR Health Readiness Inc. (formerly MEDLOG Inc.).
JVR Health Readiness is a woman-owned/ Veteran-owned Healthcare consulting and services organization dedicated to Health and Medical Readiness.
Mr.
Rush has over twenty-six years of Healthcare Materials
Management and leadership experience with healthcare and
public health organizations in both the Public and Private
Sectors. He was Middle East Regional Materials Manager with
the U.S. Air Force and later served as the Medical War
Reserves (stockpile) Manager on the Surgeon General,
Europe’s staff in Germany. He later served the Army as a
civilian employee and the Chief of Medical Material
Requirements for the Readiness division of the U.S Army
Medical Material Center, Europe (USAMMCE).
Most recently, Mr. Rush was the Region III Project Officer
with the National Bioterrorism Hospital Preparedness
Program. As a Health Resources and Services Administration
Project Officer, he provided technical assistance to HRSA
awardees in developing a truly integrated approach to
planning, training and testing their effectiveness for
managing the full spectrum of man-made and naturally
occurring disasters.
In the Private Healthcare Industry, Mr. Rush has held
positions as the Materials Manager at the Children’s
Hospital and Center for Reconstructive Surgery in Baltimore,
Maryland and at Barrow Medical Center in Winder Georgia and
as the Director of Purchasing at Garrett County Memorial
Hospital, in Oakland Maryland. He has broad experience with
Governmental acquisition systems, as well as major civilian
healthcare Group Purchasing Organizations (GPO). He
specializes in aggressive Materials Management initiatives
and the development of “Corporate Materials Management”
standardization programs. He also uses his extensive
experience in managing very large wartime and disaster
related medical materials management systems to assist
customers in developing disaster or bioterrorism materials
management programs.
Mr. Rush was the first Logistics Manager for the National
Pharmaceutical Stockpile Program at the Centers for Disease
Control and Prevention. In that capacity he developed
storage and stock rotation plans to effectively and
efficiently manage over $300 million in pharmaceuticals,
emergency equipment, vaccines, blood products and other
lifesaving commodities.
His professional papers have been published in the
International Association of Emergency Managers newsletter,
with worldwide circulation. Excerpts of his article
“Preparing for Bioterrorism” have been published by the
Materials Management magazine, a joint publication of the
American Hospital Association (AHA) and the Association of
Healthcare Resources and Materials Management (AHRMM).
In December, 2005, Mr. Rush served the Federal Emergency
Management Agency (FEMA) as a subject matter expert on a
focus group for an upcoming FEMA healthcare course. This
course will help leaders develop comprehensive healthcare
emergency management programs to manage future disasters.
This course will also highlight recent lessons learned in
disasters where healthcare organizations could no longer
sustain patient care and had to evacuate the facility. The
course will also present topics designed to help mediate or
eliminate healthcare operational vulnerabilities in future
disasters.
You can reach Jim via email at Medloginc@aol.com
Previously on Jim Rush:
A Happy
Thanksgiving Wish for Everyone Out There on the Front Line
[Nov 20 07]
The
Materials Manager's Role in Pandemic Preparedness
[Oct 26 07]
Pandemic
Planning Shortfalls - Culture of Scarcity
[Oct 8 07]
Establishing, Provisioning and Managing Special Needs Shelters
Training Citizens for Disasters [Jul 31 07]
Become a Mission Integrator [Jun 30 07]
Pandemic Planning: Why Healthcare and Public Health Aren't Talking [May 11 07]
The contents of this site, unless otherwise specified, are copyrighted by © Big Medicine 2001-2009. The news provided is for personal use only. Reproduction or redistribution of the this site, in whole, part or in any form, requires the express permission of Big Medicine or the original source. For questions or comments pertaining to this site, contact the web administrator. Big Medicine is not responsible for the content of external sites linked and does not endorse their content. Advertisers are not responsible for Big Medicine contents, the content of external sites linked and do not endorse their content.